Patients presenting to the ED with migraine pain can often present a challenge in terms of pain control. For patients who have pain refractory to NSAIDs, IV fluids, and migraine abortive therapies, or those who would prefer not to receive an IV, what other options can we turn to?
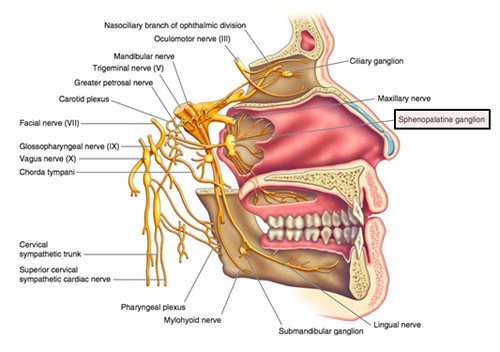
The sphenopalatine ganglion (SPG) plays a pivotal role in nociception of headache and facial pain. Recent evidence has implicated the SPG as an important neural relay point for common migraine. As activation of the SPG causes parasympathetic-mediated vasodilation of the cerebral vasculature, producing headaches, anesthetizing the ganglion is thought to attenuate this dilation, resulting in rapid relief of symptoms.
An SPG block can be performed using transnasal, transoral, and lateral infratemporal approaches but for our purposes in the ED, transnasally is the easiest and most practical of these three. To perform a transnasal SPG block, follow the following steps:
- Soak a long 10 cm cotton-tipped applicator in local anesthetic (1% to 4% lidocaine or 0.5% bupivacaine)
- With the patient’s head in a sniffing position, insert the soaked cotton-tipped applicator into the naris, on the unilateral side of the patient’s headache.
- Apply firm and steady pressure (similar to the insertion of nasal packing) along the superior border of the middle turbinate until you meet resistance at the posterior wall of the nasopharynx. At this point, the local anesthetic should contact the SPG and anesthetize the ganglion
- Leave the cotton-tipped applicator in place for 5-10 minutes, after which the patient should experience significant improvement or resolution of their headache!
What’s the evidence?
Anecdotally, there has been a positive response to SPG blocks for migraines. However, the review of the literature is mixed.
In a double blinded RCT conducted in 2 large academic EDs, a 50% reduction in pain was achieved in 48.8% of the bupivacaine group (20/41 patients) versus 41.3% in the normal saline solution group (19/46 patients), for an absolute risk difference of 7.5% (95% confidence interval [CI] -13% to 27.1%) which was not statistically significant. However, as a secondary outcome, at 24 hours, more patients in the bupivacaine group were headache free (24.7% difference; 95% CI 2.6% to 43.6%) and more were nausea free.
Another double blind RCT demonstrated a statistically significant reduction in headache with bupivacaine at 15 and 30 minutes and sustained at 24 hours for SPG blockade with bupivacaine vs saline.
It’s important to note that in both these studies, the SPG block was performed using the Tx360(®) device rather than the cotton swab technique mentioned above.
Currently, there’s not great evidence that SPG blocks are helpful and more studies are needed before this becomes standard of care for migraines. However, they do provide one more option for pain control in patients with migraines, particularly in those who don’t want an IV.
References:
Jeffrey Shih, Chris Gaafary. “Trick of the Trade: Sphenopalatine Ganglion Block for Treatment of Primary Headaches” Academic Life in Emergency Medicine Published on March 22, 2017. Accessed on July 24, 2017. Available at [https://www.aliem.com/2017/03/trick-sphenopalatine-ganglion-block-primary-headaches/]
Cady R, Saper J, Dexter K, Manley H. A double-blind, placebo-controlled study of repetitive transnasal sphenopalatine ganglion blockade with tx360(®) as acute treatment for chronic migraine. Headache. 2015;55(1):101-116.
Schaffer J, Hunter B, Ball K, Weaver C. Noninvasive sphenopalatine ganglion block for acute headache in the emergency department: a randomized placebo-controlled trial. Ann Emerg Med. 2015;65(5):503-510.
