You have just recently started a lucrative position in a small rural hospital in Northern Vermont. In your first week you are working a single provider overnight shift and a patient presents for a laceration to their left hand.
History: 25 year old right handed male, at home cutting a steak when the knife slipped and he sustained the injury below.
He has sensation in the distal left 2nd digit and good capillary refill. Motor exam reveals difficulty with full extension of the left 2nd digit. After the exam you go back to your desk and try to remember if it is orthopedics or plastics covering hand, then you remember… There is no hand.
Lacerations to the posterior hand can be complex and require complex repair. This review of extensor tendon lacerations is provided via ACEPnow.
The first step in assessing lacerations to the hand prior to closure are to rule out foreign body retention and neurovascular compromise. Then after extensive irrigation underlying tissue damage can be evaluated.
Flexor tendon injuries are not frequently repaired in the ED. It is important to achieve hemostasis/closure to prevent infection and then splint with prompt follow up.
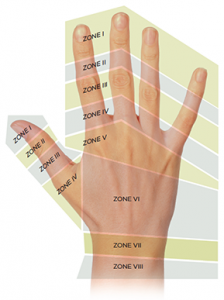
For extensor tendon injuries it is important to remember the zones of the hand.
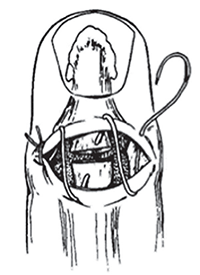
Zone I injuries: Generally closed with or without repair via the roll stitch (pictured below) and splinted in the hyperextended position at the DIP.
Zone II Injuries: Open extension injuries to the middle phalanx can be repaired by ED physicians similarly to zone 1 (roll stitch). More complex lacerations, should be splinted and have close hand surgery follow up.
Zone III Injuries: Open Lacerations involving the tendon should be closed without repair of the tendon, and splinted with 30 degrees of extension and wrist, 15 degrees of flexion at the MCP and PIP in neutral position with close specialist follow up.
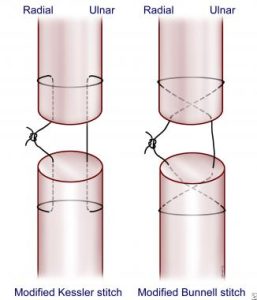
Zone IV injuries: Tendons in zone IV become larger and easier to repair. Tendons with >50% laceration can be repaired with the Kessler technique (See below). After repair patients should be splinted like zone 3 injuries and have close OP follow up.
Zone V: The fight bite region. Patients should be treated as a fight bite until proven otherwise. Irrigate, start the patient on antibiotics, splint and have return for wound check in 24 hours or to a hand specialist in the same time frame. Do not close these wounds if there is any suspicion for human bite.
Zone VI: Larger tendons in this area make for easier repair. Using the modified Bunnel technique (see below) the tendon can be repaired. Patients should then be closed, splinted with wrist in 30 degrees of flexion, all other joints neutral and the have close follow up with a hand surgeon.
Zone VII and VII: larger involvement of muscle belly makes these zones outside the scope of EM physicians. Close the wound, place patient in a volar splint and give close follow up.
Key points:
- Do not repair flexor tendon injuries, irrigate, close and splint with close follow up.
- If there is any doubt if a tendon injury is present, splint and follow up.
- In general if you are unable to repair the tendon, splint and give close (within 1 week)
- In Zone 1 injuries, patient adherence to splinting is most predictive of functional outcome.
Sources: Mcgovern, McNamee, I. “Emergency Department Management of Extensor Tendon Lacerations” http://www.acepnow.com/article/emergency-department-management-of-extensor-tendon-lacerations/2/?singlepage=1