You are once again working your solo overnight shift and Rural General Stand Alone Hospital. In the door walks a 33 yo G6P5 female with abdominal cramping who is 35 weeks pregnant. The labor and delivery service recently closed down and all OBGYN is being referred to the regional hospital 45 minutes away. The patient came in to you ER because the commute is too much for her every time she has cramping. As you are asking standard questions like how far apart are you contractions she has a precipitous delivery.
Now in front of you is a newborn infant and a screaming mother and father. Clamp/Clamp cut and you have the baby on a warmer that is luckily left over from the days when there were pediatric services at your hospital. Initial APGARs are O, the baby is grey, apneic and pulseless. What are your next steps?
The following information is from “Towards evidence-based resuscitation of the newborn infant”
http://www.sciencedirect.com/science/article/pii/S0140673617305470
Summary:
- Aggressively dry and stimulate baby
- If apneic give 6 rescue breaths and reassess
- Apply spO2 ( Pearl: Newborns still have preductal circulation so the best best place for O2 sat is on the right hand)
- If still apneic give 30 seconds of ventilation ensuring chest rise with head in proper position.
- Ask for assistance to get good 2 person seal and ventilation with ideal head position.
- Pearl: Resuscitation of newborns should start with 21% oxygen not 100%.
- If you are have trouble bagging the patient remember the mnemonic MR SOPA
- Mask has tight fit
- Re-positiong into “sniffing” position
- Suction nares and pharynx
- Open Mouth
- PPV to max of 40 cmH2O
- Alternative Airway
“Positive-pressure ventilation is arguably the most important intervention in neonatal resuscitation”
- If still apneic, pulseless or bradycardic (HR <60) start compressions
- 3:1 compressions to breaths (Pearl: Newborns are much more respiratory dependent so in 1 minute there should be 90 compressions and 30 breaths)
- Continue on to Neonatal Resuscitation Algorithm (Compressions, IV access, Epinephrine etc)
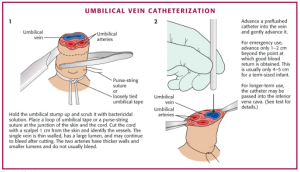
- Pearl: IV access in neonates can be achieved via an umbilical vein catheter (See image below). Tips: look for the compressible vessel, insert until there is blood return but not much further, use ligature suture or premade equipment to compress arteries. Secure in place similar to chest tube.
After 30 seconds of rescue breaths the HR has improved but is still below 60. You quickly intubate and continue NALS.
After one rounds of NALS the HR and spO2 have improved (refer to chart 1 for acceptable spO2s) and you have clear ROSC. NICU at the receiving hospital has accepted the patient and the neonate is all prepped for transfer.
Sources: Manley, B. Et al “Towards evidence-based resuscitation of the newborn infant” The Lancet VOLUME 389, ISSUE 10079, P1639–1648, 22 APRIL 2017