Clinical Question – What is the best way to intubate and provide post-intubation care for the critically ill asthmatic?
Case: 54M mhx asthma (hx of 2 intubations, last 2 months ago) presents to the cardiac room in respiratory distress. He fails nebs/steroids/mag and becomes obtunded after you trial bipap. A decision is made to intubate the patient. He is tachycardic to 110s but otherwise normotensive.
What are the best RSI agents to intubate the asthmatic?
- Induction = Ketamine – 1-2 mg/kg – preferred induction agent because of bronchodilation. In the patient that is tachypneic, anxious, and is ripping off their bipap mask, you can perform a DSI before intubation.
- Paralysis – Rocuronium 1.2 mg/kg is the preferred choice because it allows for ~ 45 minutes of paralysis, which will allow the patient to become synchronous with the ventilator after intubation.
The patient is now intubated. Don’t relax – your problems are actually just beginning.
Your patient will be hypercarbic and you will have the impulse to increase the vent’s respiratory rate in order to blow off CO2. This is the wrong move, and may kill your patient.
Physiology –
- Your patient cannot expire CO2 normally due to their bronchospasm, inflammation and mucus production. Increasing their RR will decrease the time they will have to fully exhale, therefore leading to breath stacking (CO2 literally builds up in the alveoli because it be expired) and increasing their alveolar pressures, leading to a higher chance of a pneumothorax. The increased intrathoracic pressure will promote hypotension.
How do you avoid this?
- Vent Settings for Obstructive Lung Disease: The goal is to give as much expiratory time as possible.
- Settings – AC-VC. VT 6-8 cc/kg IBW, RR – 6-8, I:E 1:4-5. Increase Inspiratory Flow Rate to Maximum. The combination of these settings will give patients maximal time to exhale. FiO2 and PEEP can be minimized because the problem is ventilation, not oxygenation. This leads to permissive hypercapnea as the steroids and nebs take their effect.
- Maintain Ventilator Synchrony – you need to ensure that the patient isn’t breathing faster than the vent. Look at the FTot at the top of the ventilator – this tells you the actual breaths the patient is taking. If the patient’s Ft is 22, then they’re breathing at 22 BPMs, which negates the effect of your ventilator settings.
- Prevent Vent Asynchrony – you’ll need to heavily sedate patients. Use an analgesia first strategy (Fentanyl/Dilaudid); add on propofol and consider precedex or midazolam as third-line if this doesn’t works. These patients may need a central line and pressors from the hypotension they get from their heavy sedation. Consider an arterial-line if you are going to be doing frequent blood gas sampling.
- If Sedation Fails, consider paralysis. This is beyond the scope of this pearl and is a strategy that may be pursued in the ICU.
- Avoid Hyperoxia – hypoxic vasoconstriction diverts blood from lung units most affected by bronchospasm. As a result, your body naturally optimizes V/Q matching. In a hyperoxic state, the poorly ventilated bronchospastic regions are getting a ton of O2. Hypoxic vasoconstriction stops, and V/Q matching worsens because the bronchospastic areas are now participating more.
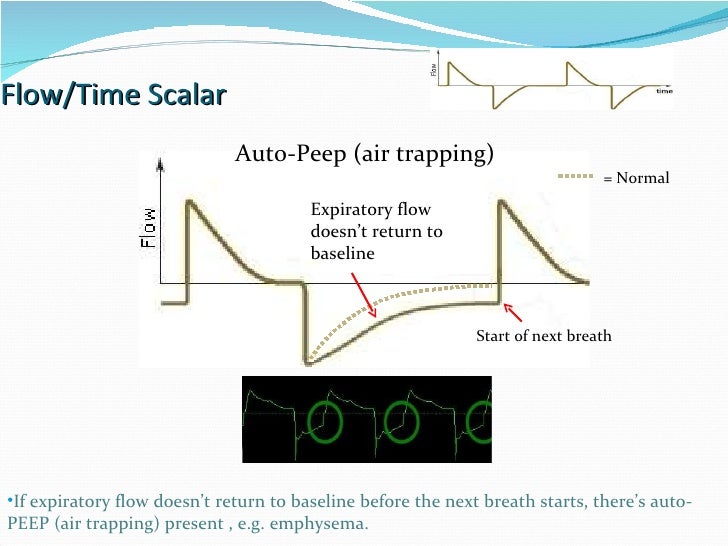
- Avoid AutoPEEP – your ventilator can tell you if the patient is breath stacking. Look at the flow-time curve. The solid line is autopeeping, and the dotted line is normal. If you are autopeeping, this is likely because your RR is too still too high. Continue dropping it.
Thanks to Dr. Angela Chen for the question.
Sources:
- Deranged Physiology – Ventilation Strategies for Status Asthmaticus
- EMCRIT – Dominating the Vent Part 2
