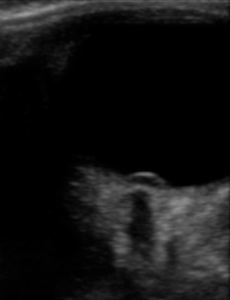
What’s abnormal in this image?
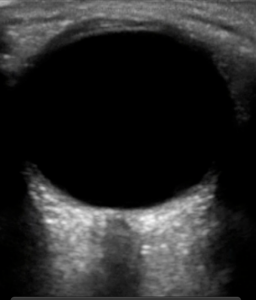
Here’s a hint. Â Here is an example of normal.
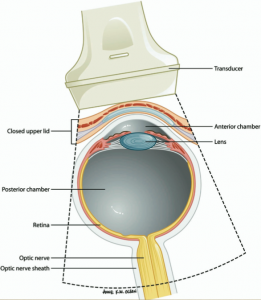
When evaluating for possible elevation in intracranial pressure, it has been shown that optic nerve sheath diameter (ONSD) measurements correlate with elevated intracranial pressures.(1,2)  The optic nerve attaches to the globe posteriorly and is wrapped in a sheath that contains cerebral spinal fluid. The optic nerve sheath is contiguous with the dura mater and has a trabeculated arachnoid space through which cerebrospinal fluid slowly percolates.
ONSD Normal Ranges
| Normal Adults | < 5 mm |
| Children >1 yr | < 4.5 mm |
| Infants < 1 yr | <4 mm |
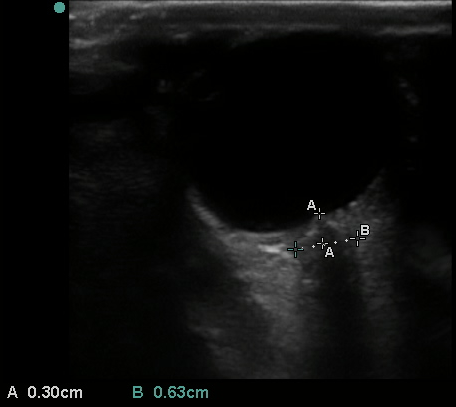
The ONSD is measured 3 mm posterior to the globe for both eyes. A position of 3 mm behind the globe is recommended because the ultrasound contrast is greatest.  It is best to average two measurements of each eye. An average ONSD greater than 5 mm is considered abnormal and elevated intracranial pressure should be suspected.
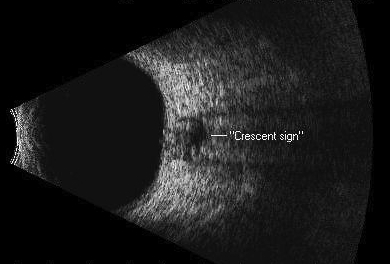
Crescent Sign
In severe cases of elevated ICP, one can see an echolucent circle within the optic nerve sheath separating the sheath from the nerve due to increased subarachnoid fluid surrounding the optic nerve.  Ophthalmologists refer to this as the crescent sign.
 The Case
40 yo female patient presents with several months of frontal headache associated with photophobia and blurry vision. Â Symptoms have gotten much worse over the last few days and she has had difficulty reading and watching TV because of her visual symptoms. Â She denies fevers, chills, nausea, vomiting, or focal weakness. Â Pt is hypertensive 170/100. Â Her vital signs are otherwise normal.
- Visual acuity -Â 20/30 OD, 20/70 OS
- CT head is normal
- Bedside point of care ultrasound
papilledema cropped from Sinai EM Ultrasound on Vimeo.
Papilledema 2 cropped from Sinai EM Ultrasound on Vimeo.
This patient had enlarged ONSD (measurements were 6 mm bilaterally) as well as papilledema(arrow).
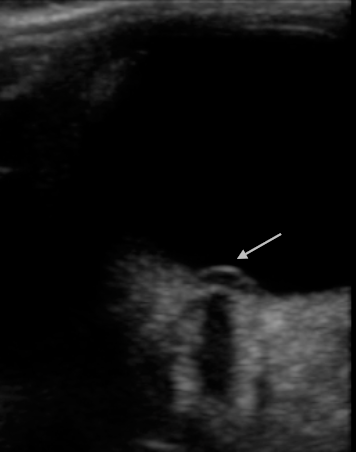
Lumbar puncture was performed. Â Opening pressure was 44. Â 30 cc’s of CSF was drained and the closing pressure was 11. Â The patient’s headache and visual symptoms improved . Â She was started on acetazolamide and admitted to the neurology service. Â MRI brain prior to lumbar puncture showed posterior scleral flattening bilaterally with protrusion of the optic nerve in the the globes bilaterally consistent with increased ICP.
This patient’s papilledema and increased ONSD correlated with a markedly increased opening pressure during lumbar puncture and suggests that ocular ultrasound may play a role in the ED management of patients with suspected pseudotumor cerebri.
Pseudotumor cerebri
Elevated intracranial pressure in the abscence of intracranial mass lesion. Most common in young, over weight women. If the diagnosis is missed, persistently elevated intracranial pressure can lead to optic atrophy and blindness.
Treatment
- Lumbar puncture to drain CSF to a normal opening pressure.
- Medical:Â Diomox (acetazolamide), high dose steroids
- Surgical : Optic nerve sheath fenestration, VP shunt
Summary
The ability to diagnose papilledema using bedside sonography is useful to emergency physicians, as many non-ophthalmologist clinicians do not feel confident in their ability to perform an accurate nondilated fundoscopic examination. (3)  Ultrasound provides a useful alternative means of determining the presence or absence of papilledema in a patient in whom fundoscopy cannot be adequately performed.
[1] Geeraerts T, Launey Y, Martin L, et al. Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive Care Med 2007;33(10):1704-11 [electronic publication 2007 Aug 1]. PMID: 17668184
[2] Kimberly HH, Shah S, Marill K, Noble V. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad Emerg Med 2008;15(2):201-4. PMID: 18275454
[3] Wu EH, Fagan MJ, Reinert SE, Diaz JA. Self-confidence in and perceived utility of the physical examination: a comparison of medical students, residents, and faculty internists. J Gen Intern Med 2007;22 (12):1725-30 [electronic publication 2007 Oct 6]. Â PMID:Â 17922165