This is a review of specific pediatric entities that may cause abdominal pain, bloody diarrhea, or vomiting. The following lists are not comprehensive and emergency physicians should consider a broad differential based on symptoms and presentation. The aim of this pearl is to familiarize us with these select pediatric conditions.

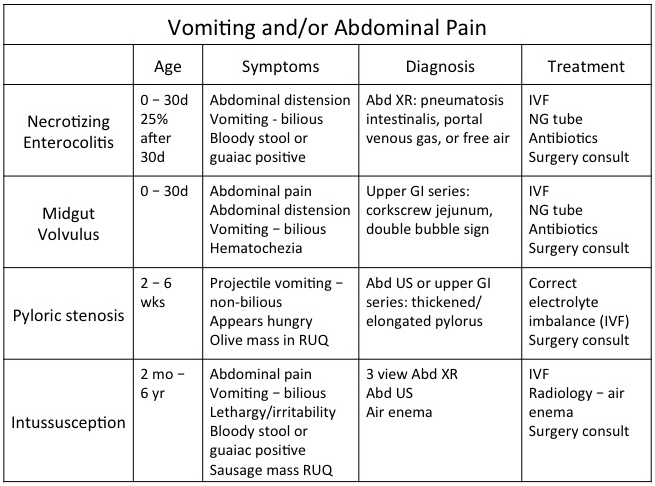
Necrotizing enterocolitis typically presents secondary to bacterial overgrowth in the bowel causing translocation of the bacterial endotoxin and gas in the intestinal wall. Risk factors include prematurity, ischemia, infection, rapid feeding, congenital heart disease, or immunocompromise. Incidence decreases with increasing gestational age and birth weight. Furthermore, presentation of symptoms is inversely related to gestational age, meaning premature infants will present later than term infants (a 26 wk premie will present at DOL 23, a 31 wk premie will present at DOL 11). Work-up includes abdominal x-ray, CBC, CMP, blood gas, coagulation panel, T&S, and blood cultures. Management includes antibiotics, bowel rest, surgery consultation, and aggressive supportive care with IV fluids. Surgery consultation is necessary as some of these patients progress to needing bowel resection.1

Midgut volvulus classically presents in the first month of life however can present later. Suspect in infants with bilious emesis or feeding intolerance. Pain and irritability may not be present in the neonate. The abdomen is usually soft and non-tender until strangulation of the bowel. After strangulation of the bowel one can see abdominal distension and hematochezia. Once the bowel is necrotic the infant can rapidly deteriorate and present in shock. Pediatric surgery consultation for emergent surgical correction is imperative.2
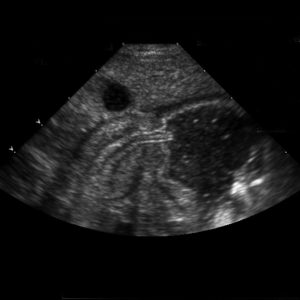
Pyloric stenosis presents as a gradually worsening vomiting post-feeds. If the child has severe pyloric stenosis and is PO intolerant they may have electrolyte abnormalities such as hypochloremic metabolic acidosis. For this reason, work-up can include electrolyte and blood gas measurements. Diagnosis is obtained through abdominal ultrasound or upper GI series. If it is off-hours for imaging, well appearing children who can tolerate PO with no electrolyte abnormalities may be sent home if outpatient/ED follow-up is prompt (next day) and guardians are reliable. Definitive management with pediatric surgery for a pyloromyotomy.3
Intussusception
See post on December 23 for symptoms and work-up. Management consists of air enema for decompression or surgery.
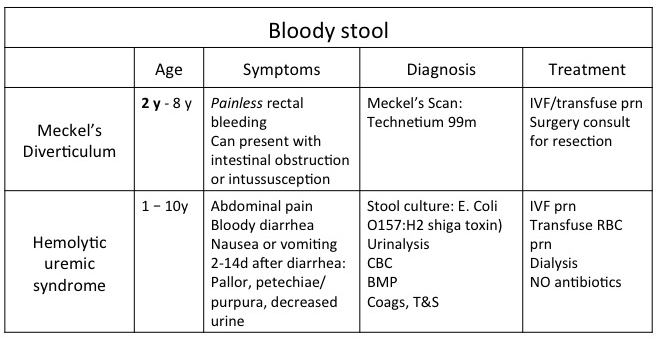
Hemolytic uremic syndrome is a triad:
- Microangiopathic hemolytic anemia
- Thrombocytopenia
- Acute renal failure
The most common etiology of this syndrome is shiga toxin secondary to E. coli O157:H7. HUS is the most common cause of acute renal failure in the pediatric population. Transfusion of platelets is contraindicated as the thrombocytopenia can become consumptive. 4
Meckel’s diverticulum is best remembered by the rule of 2’s:
- 2% of the population
- Male-to-female ratio 2:1
- 2-years-old
- Found within 2 feet of the ileocecal valve
- 2 inches long
- 2% develop complications (hemorrhage, obstruction)
Diagnosis is with nuclear medicine technetium 99m scan. If it is off-hours for imaging, well appearing, hemodynamically stable children may be sent home if outpatient/ED follow-up is prompt (next day) and guardians are reliable. Ultimately these children require pediatric surgery consultation for excision of abnormal tissue.5,6
References
- Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011;364(3):255-264.
- Marin JR, Alpern ER. Abdominal pain in children. Emerg Med Clin North Am. 2011;29(2):401-428, ix-x.
- Paul RI. Pyloric Stenosis. In: Schafermeyer R, Tenenbein M, Macias CG, Sharieff GQ, Yamamoto LG, eds. Strange and Schafermeyer’s Pediatric Emergency Medicine, 4e. New York, NY: McGraw-Hill Education; 2015.
- Razzaq S. Hemolytic uremic syndrome: an emerging health risk. Am Fam Physician. 2006;74(6):991-996.
- Pershad J, Huang EY. Meckel's Diverticulum. In: Schafermeyer R, Tenenbein M, Macias CG, Sharieff GQ, Yamamoto LG, eds. Strange and Schafermeyer’s Pediatric Emergency Medicine, 4e. New York, NY: McGraw-Hill Education; 2015.
- Sagar J, Kumar V, Shah DK. Meckel’s diverticulum: a systematic review. J R Soc Med. 2006;99(10):501-505.