This pearl is based off a question on our in-service yesterday.
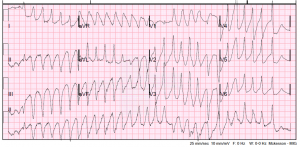
You are working resus and a 63 yo M presents with altered mental status. He has a LVAD. His EKG is below:
Time to call the LVAD team right? Well what if you can’t reach them or you receive this patient in a small community hospital without a LVAD team, what will you do? Since these devices are becoming more common, emergency physicians should have a basic understanding of how to manage the complications.
There are three main principles surrounding LVADs:
1) The RV is not supported and derangements in the physiology of your LVAD can severely affect your RV and cause it to fail.
2) The LV still functions but is greatly supported by the LVAD. However, pump failure or LV failure will cause backup and ultimately RV failure and collapse.
3) The LVAD is basically a vacuum and sucks blood of out the LV and unloads it into the aorta; it is dependent on preload and afterload.
Obtaining a BP is crucial in understanding the physiology of these patients. There are numerous sites, which discuss the mechanics of obtaining a BP in these patients listed below. To simplify this, either obtain a MAP with aid of an ultrasound or place an arterial line.
The other things to address are those numbers on the LVAD machine. We need a simple understanding of these parameters as discussed below. Current settings will be compared to normals (which are set by the CT surgeon), which your patients will know.
Pump speed (RPM): This is how fast the rotor is spinning and is typically between 6000-10,000 rpms. This essentially is the patient’s Cardiac Output.
Power (watts): This is the electrical current required to maintain the pump speed. This should not vary much and if it is changing may help you recognize pathology.
Flow (L/min): A calculated estimate of the cardiac output.
Pulsatility Index: This is the most confusing parameter. Essentially this is a measure of the amount of work or contractility of the L ventricle. As the PI decreases, the LV is working less (and smaller in size )and your MAP is becoming more dependent on the pump. If the PI is increasing, the LV is proportionally increasing its workload to maintain your MAP (and has increased in size).
With this knowledge we can address LVAD emergencies.
Suction Events: The pump is dependent on preload. It will continue to suck blood from the ventricle to maintain cardiac output. If a patient is hypovolemic the pump can actually suck down the ventricular wall/septum. This will be represented by a decrease in the power (since the pump has less volume to move) and changes in the pump speed as the pump tries to autoregulate this problem. The PI will also decrease with hypovolemia. Thrombi in the inflow or outflow tract will also precipitate similar events but should not change the PI. So if your power is decreasing and the pump speed is variable consider hypovolemia vs inflow/outflow thrombus and give IVF/blood and/or anticoagulate.
Rotor Thrombus: Another common occurrence is the development of a thrombus in the actual rotor. If this occurs you will note increasing power to maintain a constant pump speed, increased PI and may receive alarms regarding low flow. Other clues will be an increase in LDH, hematuria and worsening renal function. The treatment for this will be anticoagulation.
Ventricular Arrhythmias: These patients have sick hearts and are prone to dangerous arrhythmias including vtach/vfib. The above problems can also precipitate these arrhythmias. The problem with these arrhythmias is they can lead to hypotension and RV failure if ignored. LVAD parameters will show decreased power and decreased PI. If your patient is hypotensive or showing clinical signs of hypotension (AMS) with a dangerous ventricular rhythm, the answer is cardioversion. If the patient is stable, consider anti-arrhythmics such as Amiodarone or Lidocaine.
- http://emcrit.org/wee/left-ventricular-assist-devices-lvads-2/
- http://www.emdocs.net/lvad-patients-what-you-need-to-know/
- http://lifeinthefastlane.com/ccc/ventricular-assist-device/
- http://www.christem.com/eruditionem/2014/1/3/left-ventricular-assist-devices.html