During a busy day in the ED, it becomes apparent that the pulling and yanking on your patient’s shoulder has done absolutely nothing to reduce their shoulder. You perform your pre-procedure PSA Checklist, know that this young and active 18 year old poses little difficulty, and push your desired dose of ketamine.
Suddenly, you notice the Oxygen Saturation dropping….98….92. You see chest rise but begin to hear stridor. What happened? What can you do to intervene?
Laryngospasm.
This is one of the rare but feared complications of procedural sedation. It recognizes rapid and immediate intervention to prevent rapid clinical deterioration. Complications include: desaturation, pulmonary edema, organ ischemia, cardiac arrest.
Here are the things you can do to help relieve laryngospasm:
- Be prepared for emergent intubation
- Suction or clear the airway if there is any physical obstruction present
- Manual ventilation via BVM and a PEEP valve. Positive pressure is essential when trying to combat laryngospasm
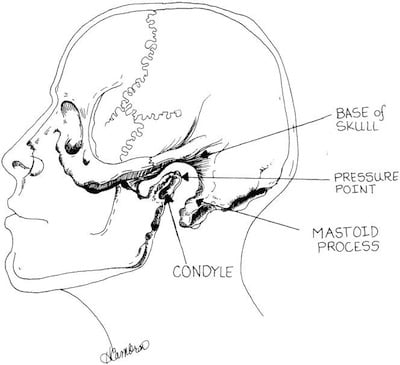
- Put pressure on the laryngospasm notch (Larson’s Point) while performing a jaw thrust- this is an extremely painful pressure point which can provide the sympathetic surge to help break the spasm.
If all of this has been done but the patient is still difficult to ventilate, you may administer succinylcholine. Though this is not your intubating dose— you give 0.1-0.5 mg/kg. Beware that as the medication wears off, spasm may recur.
Below you will find: A Comprehensive PSA checklist by Drs Strayer and Andrus, an image of laryngospasm, and a diagram demonstrating Larson’s Point:
https://emupdates.com/perm/PSAChecklistv2emupdates.com_print.pdf