This series is designed to discuss topics that we might not routinely encounter during our training or how to manage patients we would normally triage to a sub-specialty service.
This pearl comes courtesy of an excellent review on emDoc. “Cystic Fibrosis ED Management Pearls and Pitfalls” http://www.emdocs.net/cystic-fibrosis-ed-management-pearls-pitfalls/
Basic Pathophysiology:
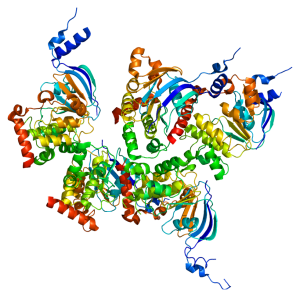
Cystic Fibrosis (CF) is an autosomal recessive disease that can affect multiple organ systems. Many people remember back to medical school when we learned that CF is a mutation in the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) which is a chloride channel. The general consequence of this mutation is that mucous and exocrine glands have decreased ability to secrete chloride. This generally affects the lungs, intestines, biliary system and pancreas.
Acute Pulmonary Disease:
- Special considerations:
- In CF patients 85% of mortality is due to progressive pulmonary disease.
- CF patients have chronic lung infections leading to persistent cough and obstructive lung disease. Most pulmonary exacerbations are triggered by expansion of colonized strains of bacteria, not newly acquired infections.
- Spontaneous pneumothorax is more common in older patients and those with advanced disease.
- Trace/Minor hemoptysis is common, does not always require extensive workup
- Pneumonia: Staph Aureus and Haemophilus Influenzae are common early in life. Pseudomonas once colonized is functionally impossible to eradicate. In general management is with high dose antipseudomonal (aminoglycosides + B-lactams) but ideally should be tailored off of the patient’s last sputum culture.
- Allergic Bronchopulmonary Aspergillosis (ABPA) should be kept in the differential for wheezing CF patients. Diagnosis of ABPA is not commonly made in the ED but the treatment is steroids.
- General management
- Inhaled hypertonic Saline is beneficial in acute exacerbations when followed with chest PT.
- Bronchodilators have an unclear efficacy but have a benign risk profile so may be considered. They are more effective when dosed immediately before hypertonic saline.
- NIV: Observational studies show that NPPV may be useful in acute CF exacerbations.
- According to the CF Foundation there is insufficient evidence to recommend use in an acute exacerbation.
- Antibiotics as mentioned above.
Coagulopathy:
- Patients with CF have chronic vitamin malabsorption. When bleeding is part of their presentation an INR should be checked due to Vitamin K deficiency.
Acute GI disease:
- Distal Intestinal Obstruction Syndrome (DIOS) is a pathology unique to CF patients. It is a partial or complete obstruction at the ileocecum by fecal material. It is more common in adult patients and presents as abdominal pain, usually located in the RLQ. This mass can generally be palpated due to its large size and can been seen as “granular” or “bubbly” stool on plain film x-ray. These can generally be managed with PO therapy.
SOURCE: Tassin, S. et al “Cystic Fibrosis Pearls and Pitfalls” http://www.emdocs.net/cystic-fibrosis-ed-management-pearls-pitfalls/