Happy 4th of July!
I’m taking the day to review a commonly incurred injury on the holiday: burns. Whether it’s from operating a grill after a few too many libations or an unfortunate encounter with fireworks, the incidence of burns seems to go up dramatically on the 4th.
While we mostly see minor burns in the ED, today we’ll review a systematic approach to major burns. While the definition of what constitutes a major burn varies amongst authors, the general thought is any burns requiring fluid resuscitation, involve the airway, or meet Burn Center transfer requirements are major burns. Major burns should be treated like any trauma using the ABCDE approach. However, there are some special considerations that you should think of when managing these patients.
Airway
Don’t forget to look for stigmata that may suggest burns to the airway such as singed facial hair, soot around the nose or mouth, voice changes, stridor or concern for smoke inhalation based on the clinical scenario. Assess the neck for burns or swelling as this can quickly deteriorate to an edematous and difficult airway. This should prompt early intubation. Keep in mind however, these signs of airway involvement should only move you to intubate in the case of major burns, particularly with soft signs such as singed facial hair.
Breathing
Assess for constrictive chest burns that may restrict breathing. Patients with major burns may also be at risk of cyanide or carbon monoxide poisoning.
Circulation
Patients with major burns need large volume fluid resuscitation. Shock can develop very quickly in these patients due to increased vascular permeability and developing edema, especially if they have more than 15% of their body surface area (BSA) involved. Generally, adults with >15-20% of total BSA involvement and children with >10% total BSA should receive fluids.
To calculate their fluid resuscitation needs, you’ll first have to calculate the %BSA. There are multiple ways to do this, one common method being the rule of nines, best illustrated with the diagrams below.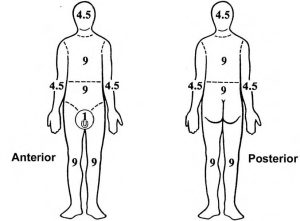
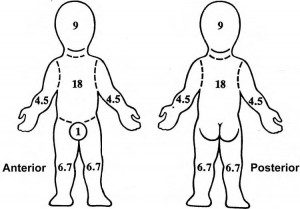
Keep in mind children have larger heads and smaller legs than adults so those areas contribute more and less to total BSA. Alternatively, you can use palmar surface to calculate BSA by remembering that the patient‘s palmar surface, palm and fingers, is approximately 1% of their TBSA. In large burns, it may be easier to use this to calculate the percentage of the unaffected areas. Finally, remember that epidermal depth burns are NOT counted in the TBSA.
After calculating the TBSA, then use the modified Parkland formula to calculate the patient’s fluid needs.
Fluid requirements for the first 24 hours = 4ml x TBSA (%) x body weight (kg)
50% given in the first 8 hours
50% given in the next 16 hours
Disability
Patients may be altered due to cyanide or CO poisoning. Poor cardiac function or an elevated lactate can be clues to cyanide poisoning, and if there is any suspicion for CO poisoning, the patient should be started on 100% O2 via non rebreather.
Exposure
Fully undress the patient as the skin exam is obviously crucial in a burn victim. Make sure to remove any jewelry and burnt or wet clothes as they are a nidus for infection. It’s also incredibly important to do a full secondary survey as patients who have suffered from burns are also at risk for suffering other trauma and the burn can distract from other injuries. Patients may be intubated or focused on the pain from the burn and unable to tell you about pain in other areas; therefore, you should be vigilant about testing all of the patient’s compartments for compartment syndrome. Patients may not need circumferential burns to develop compartment syndrome as the aggressive fluid resuscitation as well as the systemic inflammatory response can cause compartment syndrome even in unburnt limbs.
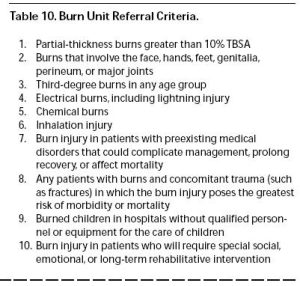
Here’s the list of burn center referral from the American Burn Association. While these are not universally accepted, they provide a good guide to when patients should be transferred. When in doubt, contact your regional burn center as they are usually more than happy to provide guidance on treatment and management of a burn patient.
Finally, don’t forget that major burn victims should be treated like any other major trauma that rolls into your ED. Patients who suffer major burns are at risk for other injuries and a full trauma assessment should be done. Don’t let the burn distract you from other potentially devastating traumatic injuries – cspine injuries, tension pneumothorax, intraabdominal hemorrhage and the like.
Happy Independence Day! Stay away from homemade fireworks!
LITFL: Trauma! Major Burns
Core EM, Podcast 101.0 Major Burns
Hettiaratchy S, Dziewulski P. ABC of Burns: Introduction. BMJ 2004; 328: 1366-8. PMID: 15178618
Guidelines for the Operation of Burn Centers (pp. 79-86), Resources for Optimal Care of the Injured Patient 2006, Committee on Trauma, American College of Surgeons