Quick word:
Demonstrating a normal sized RV does not rule out PE. With that said, if you have a hypotensive patient in whom you are concerned about massive PE, demonstrating the patient has a normal sized RV can lead you to consider alternate dangerous diagnoses.
RV size
The ratio of RV:LV chamber size should be less to 1:1. If the RV is larger than the LV, it is dilated. There’s more nuance to chamber size assessment, but for our purposes in the ED a comparison of RV:LV chamber size will work. Chamber size is best assessed from the apical 4 chamber view. The clip below is an apical 5 chamber (there’s a little of the LVOT coming into view, but this works fine). The RV is on the left hand of the screen, and is larger than the LV.
RV volume/pressure overload
As RV and LV share the fixed volume of the pericardium. The RV dilates when faced with increased afterload. With no place for that new increased RV volume to go, the RV pushes the septum into the LV. The result is a “D” shaped septum. When the LV gets compressed, LV preload falls, systemic cardiac output falls, the RV stops getting perfused, and RV contractility falls even further. This is the death spiral of RV failure.
Septal flattening in diastole suggests volume overload, while septal flattening in systole suggests pressure overload. This distinction probably isn’t important in the Emergency Department; if you see a flat septum, be cautious administering fluids.
RV function
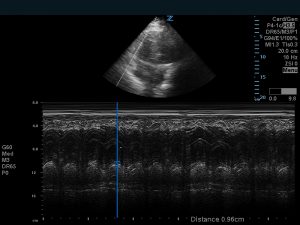
RV function is challenging to assess. Speaking for myself, this assessment leaves my comfort zone with bedside echo. The “McConell’s sign” is decreased function of the mid-RV free wall with apical sparing. If you identify a McConnells-esque RV you should be concerned. “Tricuspid annular plane of systolic excursion,” or TAPSE, uses the distance the lateral tricuspid annulus moves during systole as a proxy for RV function. A measurement of less than 1.6 cm (this number varies depending on which study you read) indicates RV systolic dysfunction. To obtain this measurement place an M mode cursor over the lateral tricuspid annulus, and measure the distance the echo-density of the tricuspid annulus moves (peak/trough). TAPSE is not a perfect measurement; I’ve found it hard to get the motion of the lateral tricuspid annulus to run parallel to the M mode cursor (leaving you to underestimate RV function). With that said, it’s worth knowing this is out there.
Pulmonary pressures
You can assess pulmonary pressures by interrogating a tricuspid regurgitation jet with continuous wave doppler; I’ve posted about the mechanics of this here.
References:
Rudski, Lawrence G., et al. “Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography: endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography.” Journal of the American Society of Echocardiography 23.7 (2010): 685-713.