Article Citation: Moore EE, Knudson MM, Burlew CC, Inaba K, et al; WTA Study Group. Defining the limits of resuscitative emergency department thoracotomy: a contemporary Western Trauma Association perspective. J Trauma. 2011 Feb;70(2):334-9. PMID: 21307731
Resident Reviewer: Courtney Cassella
What we already know about the topic:
Resuscitative ED thoracotomy (EDT) is a resource intense procedure with limited application. Prior guidelines were based on retrospective analysis. Selection of candidates was based on mechanism and duration of prehospital CPR.
Why this study is important:
This study helped update guidelines for the use of EDT. Importantly, prior to this study it was felt there was no role for EDT in blunt trauma. These guidelines select patients who may survive their trauma if given this intervention while minimizing futile care.
Brief overview of the study:
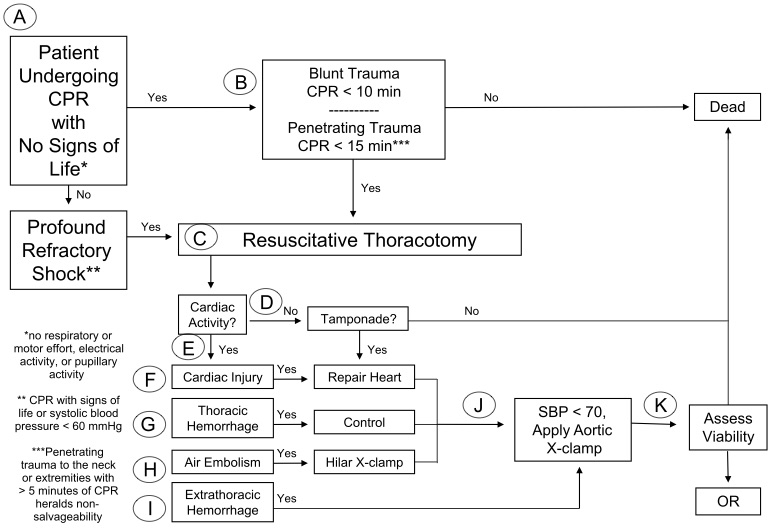
This was a prospective data registry of patients who received resuscitative thoracotomy in the ED at 18 United States Level 1 trauma centers. The decision to perform an EDT was based on duration of prehospital cardiopulmonary resuscitation (CPR) and presenting cardiac rhythm. There were 56 patients who survived to hospital discharge; mechanism of injury was stab wound (30), gunshot wound (21), and blunt trauma (5). Of the study group, 34% underwent prehospital CPR. Study survivors received CPR for less than 15 minutes in penetrating trauma and less than 10 minutes in blunt trauma, with the exception of 3 survivors. Of the 7 survivors presenting in asystole, all had pericardial tamponade.
Limitations:
- Although a multicenter registry, the sample size was small. To the author’s credit, minimal statistics were applied to this sample size. However, small sample size may exaggerate the estimated magnitude of the effect.
- The indications for ED thoracotomy were not defined between all sites. Institutional policies for ED thoracotomy were allowed. This allows for some selection bias.
- Despite efforts to standardize selection criteria, the study was not able to determine if initiation of CPR by EMS was appropriate. This also allows for selection bias.
- The study sites were Level 1 Trauma Centers that may limit generalizability to community hospitals.
Take home points (less than 50 words)
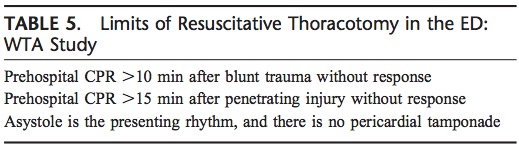
- ED thoracotomy can be considered futile when
- Prehospital CPR > 10 minutes after blunt trauma
- Prehospital CPR > 15 minutes after penetrating trauma
- Asystole as the presenting rhythm with no pericardial tamponade
West Trauma Association 2012 Algorithm1
East Association for the Surgery of Trauma 2015 Guidelines2
- Penetrating Thoracic Trauma
- Signs of life -> EDT strongly recommended
- Absent signs of life -> EDT conditionally recommended
- Blunt Trauma
- Signs of life -> EDT conditionally recommended
- Absent signs of life -> Conditionally recommend AGAINST EDT
- Penetrating extra-thoracic trauma
- EDT conditionally recommended
- Signs of life: Pupillary response, spontaneous ventilation, presence of carotid pulse, measurable or palpable blood pressure, extremity movement, or cardiac electrical activity
Additional References
- Burlew CC, Moore EE, Moore FA, et al. Western Trauma Association critical decisions in trauma: resuscitative thoracotomy. J Trauma Acute Care Surg. 2012;73(6):1359-1363.
- Seamon MJ, Haut ER, Van Arendonk K, et al. An evidence-based approach to patient selection for emergency department thoracotomy: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015;79(1):159-173.
