Let’s talk about large bore/central vascular access!
We’ll review different kinds, their different names, and when to use them!
Of note outside the scope of this review: how to insert each of these – I think this is better learned by watching videos, watching others, & doing with guidance.
This is also by no means a comprehensive vascular access guide – this is a framework to highlight three commonly used types of central lines in the ED.
Which kit do I grab to put these lines in? I included pics of each kit below from the Elmhurst trauma bay.
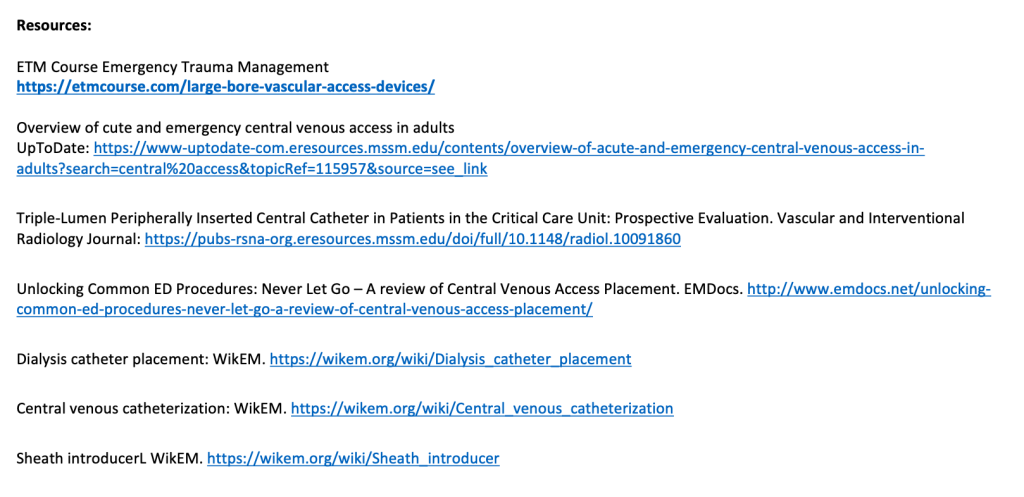
First of all, what actually makes a veinous catheter “central”? Central means the tip of the catheter is in the SVC, the IVC, or the junction between the vena cava and the right atrium (cavoatrial junction)
Three common ED central veinous access types:
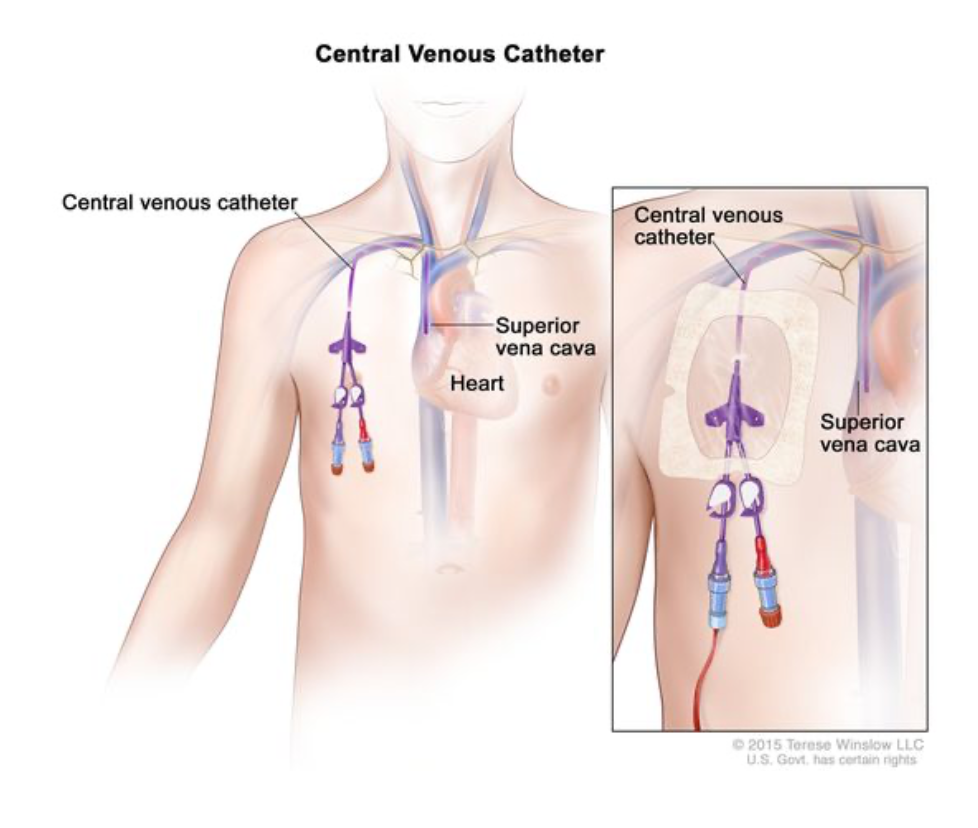
Type #1: Sheath introducer (aka large-bore introducer sheath)
What it looks like:
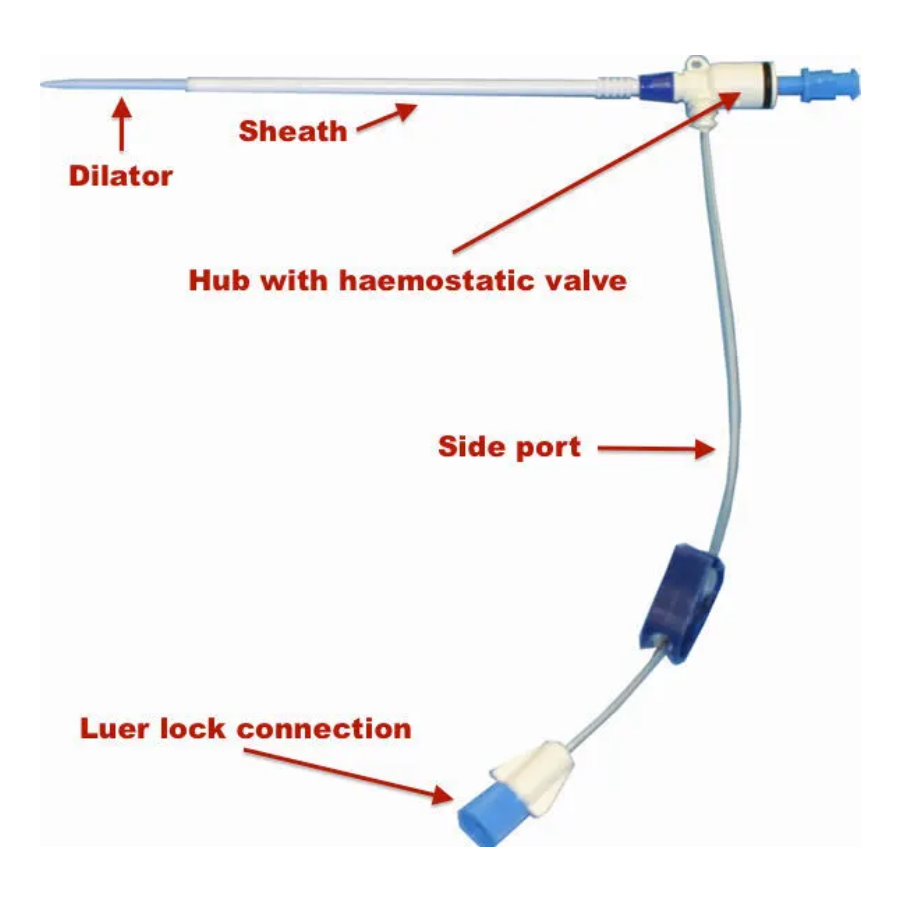
What kit to reach for:
(PSI = percutaneous sheath introducer)
The terminology:
Commonly referred to as:
- Cordis
- MAC
- Swann sheath
- Angiography sheath
How it got it’s name as a sheath introducer:
The hub serves as a “sheath” around other catheters: provides a protected portal for the catheters to enter a vessel while also allowing simultaneous allowing for fluid or med admin from the side-port/side-catheter (which runs perpendicular to the sheath).
This is why the side-port has standard luer-lock connection for IV sets to be connected, but the main sheath does not!
Common brands: Cordis, Arrow, Oscor
In the US, it’s common for for any sheath introducer to colloquially be called a “Cordis”
(Fun fact: in Australia they commonly say “Swann sheaths” instead just since they’re used to place Swann-Ganz catheters).
What it is:
A wide bore, long single lumen catheter that consists of a hub with a one-way valve, and a side port that extends to the side
Hub: port for intravascular entry: can place additional catheter or transvenous pacer through it – The one-way valve prevent backflow of blood.
– The main hub can be used to insert: triple lumen catheter, transvenous cardiac
pacemakers and pulmonary artery catheters (aka Swan-Ganz or right heart catheter) – Something cool: during coronary angiography: many angio and stenting catheters are inserted and withdrawn through the sheath. Of note during angio procedures
these can go into radial or femoral arteries.
– Using the sheath aspect prevents multiple skin punctures/introduction of bacteria
Side port: for rapid admin of blood products, IV fluids, or other meds
Of note: IV fluids (including blood) can ONLY be administered through the side port tubing via a luer lock connection. Fluid cannot be administered via the main hub.
When to use it:
Hemorrhagic shock:
Commonly used for rapid blood (or fluid) administration, often in trauma
-can infuse around 600 cc/min with pressure
Also for transvenous pacing: in the case of unstable bradycardia that is not temporized with transcutaneous pacing
Example of when to use: picture your active GI bleeder, tachycardic, hypotensive, too clamped down peripherally to get those 18-gage’s in peripherally, lab is calling you for their hemoglobin of 2 – needs a ton of blood resuscitation and needs it fast.
Sizing: can range in size from 4Fr to 11Fr (humongous) and length from 5.5cm to 23 cm. Standard mid-range size for trauma resuscitation is around 8Fr (the ones at Elmhurst for example are 8.5Fr)
Pros:
Large access with very high flow rate (lower flow rate if another catheter placed through the sheath such as a central line) to allow you to rapidly infuse fluids – often blood on our case, through them.
Cons:
Same as with any central access device, include bleeding, air embolism.
Pro tip if you ever have to remove one of these after placement: help prevent air embolism by using an obturator (blue twist-lock cap) or sterile gloved finger over the hub & apply an air-tight dressing 24-72 hours post-removal.
Type #2: Multilumen catheter
What it looks like:

What kit to reach for:
The terminology:
Commonly referred to as: Triple lumen catheter (TLC), central line, central veinous catheter (CVC)
Example brand: Arrow
What it is:
Probably the most common type of central venous access we use. This is our “bread-and- butter” central line.
Though single and double lumen catheters are available, most common is the triple lumen It is a catheter with multiple access ports that merge into a single catheter.
When to use it:
Allows administration of medications/solutions that can potentially damage or sclerose peripheral vessels or cause peripheral damage if they extravasate out of the blood vessel into surrounding tissue.
Examples of such infusions include vasopressors and hypertonic solutions
Can be used for: administering multiple meds and infusions at once, central venous pressure monitoring, emergency venous access, inability to get peripheral IV access, repetitive blood draws
Note: you can start a patient on vasopressors peripherally relatively safely as long as you have good peripheral IV access; consider switching to central line when you anticipate the patient will require ongoing vasopressor use for an extended period of time or starting centrally when peripheral access is suspect.
Example of when to use: picture your septic nursing home patient who has an EF of 30% cannot handle much fluid resuscitation, MAPs <65. MAPs improve with starting norepinephrine. The patient will be boarding in the ED a long time and has poor peripheral veins.
Sizing: usually 7Fr in diameter Depth: +/- 2 cm for each:
R IJ: 13 cm
R subclavian: 15 cm
L IJ: 15 cm
L subclavian: 17 cm
Type #3: Temporary hemodialysis catheter
The lingo:
Commonly referred to as: Shiley (this is a type of temporary HD catheter) Types include: Shiley, Quinton, Niagara, Trialysis
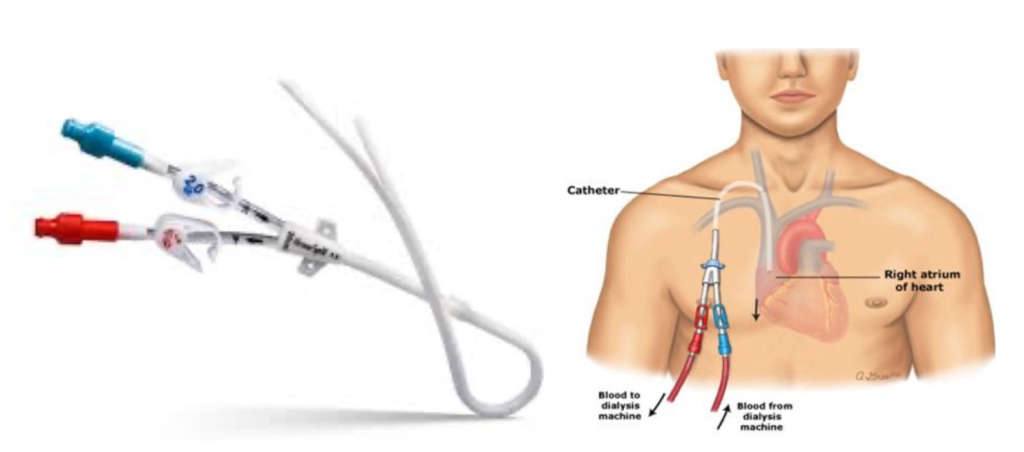
What it looks like:
What to reach for:
What it is: a two-port catheter solely for the purpose of hemodialysis
(sometimes these can come with a third port through which meds can be given: Trialysis catheter)
Two lumens:
Red = “arterial” = carries blood away from patient to HD machine
Blue = “venous” = carries blood from HD machine back to patient
When to use it: when a patient requires access for emergent dialysis “AEIOU” mnemonic for emergent dialysis indications:
A: acidosis that is severe/refractory to medical management
E: electrolyte derangement: severe, including medically refractory hyperkalemia
I: Ingestion: severe or otherwise untreatable overdose with drugs that are dialyzable (examples: methanol, ethylene glycol, lithium, salicylates)
O: overload of volume (hypervolemia) refractory to medical management
U: uremia
Sizing: these are wider in diameter than the triple lumen central (requires more dilation of the vessel). Commonly 12-14Fr.
Length varies by insertion site: R IJ: 12-15 cm, L IJ: 15-20cm, femoral: 19-24cm
Generally, preferential insertion site: RIJ>LIC>femoral>subclavian
R IJ: use 13.5Fr, 15cm catheter generally
L IJ: use 19.5cm usually
Femoral: use longest possible catheter to ensure tip reaches distal IVC
Feel: the tubing itself tends to be more firm and unforgiving than TLC: insert extra cautiously
Other helpful stuff:
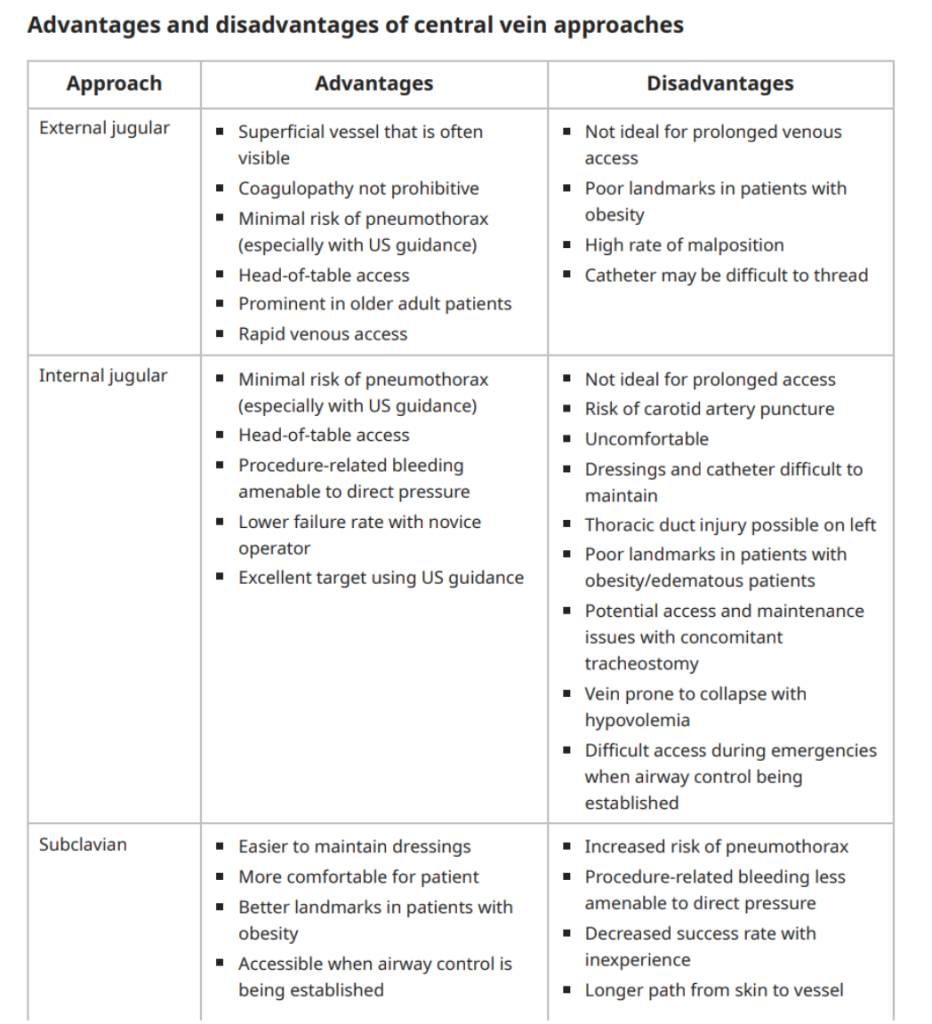
Which access site to use? – a nice table of pros and cons of each site from UpToDate here:
What are the different flow rates of these lines?
Taking us back to physics – for you nerds out there, this is the Hagen-Poseuille equation – the larger the diameter and shorter the tube, the faster the flow rate.
PIV
- 16G IV: 13.2 L/hr
- 18G IV: 6.0 L/hr
- 20G IV: 3.6 L/hr
Central Line
- 5 Fr PICC/Port: 1.75 L/hr
- 7 Fr TLC 16G distal port: 1.9 L/hr
- 7 Fr TLC 18G proximal port: 3.4 L/hr
- 12 Fr HD: 23.7 L/hr
- 8.5 Fr Cordis/introducer sheath: 7.6 L/hr
- 8.5 Fr Cordis/introducer sheath with pressure bag: 20.0 L/hr
(Interesting to note than at 18G PIV gets us kinda close for flow rate but not quite to a Cordis.)
Hopefully now you’ll feel more comfortable in deciding which LINE is SUBLIME for your patient. Happy central lining.