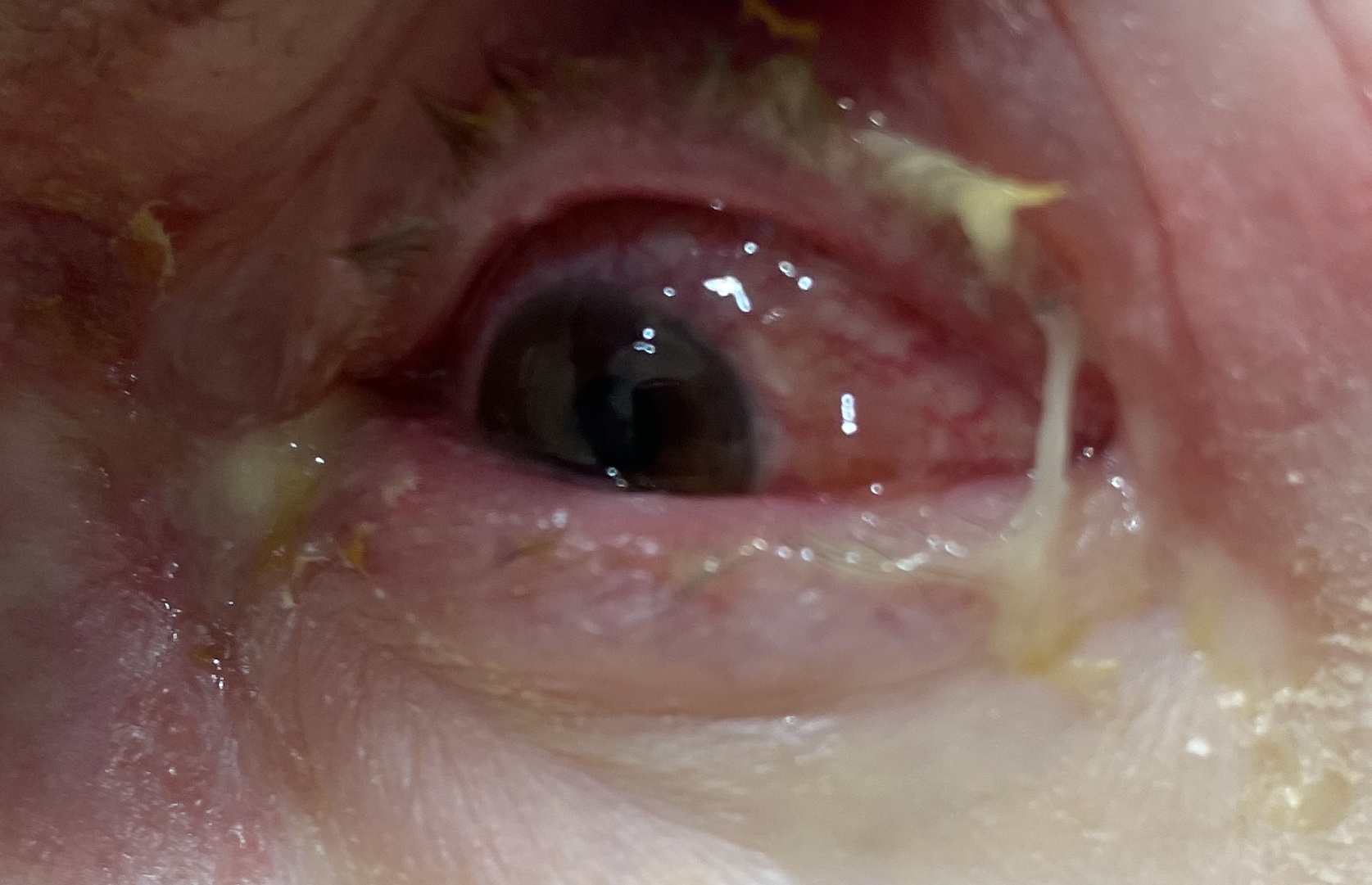
What do you think is going on here?
So if you were the resident who signed up for this patient what would you do?
As may be obvious, this is herpes zoster ophthalmicus, which is a reactivation of the VZV in cranial nerve V ophthalmic division. It’s a can’t miss visual diagnosis. Patients most at risk for this include:
- Older
- Immunocompromised like transplant patients, AIDs, malignancy
- Chronic kidney and lung disease
Zoster more generally presents in dermatomal distribution from a reactivation in a dorsal root ganglia. Patients will usually experience a prodrome of burning, stabbing pain followed by the eruption of vesicles overlying the erythematous skin. As someone who’s suffered from zoster (Covid stress was real), I can personally attest to the pain.
When the eye is involved in herpes zoster ophthalmicus, it’s important to do a thorough eye exam including:
- Visual acuity
- Extraocular eye movements as palsy can be present
- Tonometry
- Flipped lids
- Slit lamp with fluorescein looking for conjunctivitis, corneal involvement, uveitis
Slit lamp exam can show fluorescein uptake as seen below in what is known as a dendritic lesion:

Common features for eye involvement include eye pain, redness, blurred vision, fevers. Patients may also have purulent discharge around the eye. Many patients will get involvement of the nasociliary nerve producing the classic Hutchinson sign at the tip of the nose. So if you see zoster at the tip of the nose, remember to do a thorough eye exam even if the patient isn’t complaining of anything.
Management zoster in this patient involves getting our consultants onboard. We’re very lucky to have amazing consultants in house at Sinai, Elmhurst and BI but we need to be doing a thorough exam prior to calling our consultants.
Treatment should be started within 72 hours of symptoms. Patients should get an antiviral medication like acyclovir (800 mg PO five times daily) or valacyclovir (1 g PO TID). Remember that valacyclovir can be dosed every 8 hours than acyclovir which needs to be taken five times a day but acyclovir is preferential in children (dosed 20mg/kg up to 800 mg) and pregnant women. (Having tried to remember to take acyclovir myself 5 times a day, it’s pretty difficult). Patients may need to be started on IV medications if they can’t tolerate PO or have more disseminated involvement. Active lesions may also benefit from topical erythromycin and dry eyes should be lubricated if there is corneal involvement. Ophtho might start topical steroids for keratitis or uveitis. Remember to counsel patients to complete their 10 day course of treatment and of course, treat their pain. Expectation management is very key. (Zoster more generally really does hurt and itch and I still have the scars to prove it.) Medications like gabapentin or amitriptyline can really help. Also remember to council your patient on proper isolation away from at risk populations (elderly, babies, pregnant people, immunocompromised), and in the hospital they should be placed on airborne and contact precautions.
What happened to this patient?
Ophthalmology saw this patient and confirmed their vision as 20/20 in the left eye (same as the astute resident who saw the patient). Patient was started on Valtrex 1g TID with erythromycin ointment on all vesicles throughout the lid and forehead. Erythromycin ophthalmic ointment was added to the eye as well.
Symptoms worsened over the next 2 days, so the patient was started on pred forte QID in clinic which improved symptoms over the next 3 weeks.
Expert tip from ophtho: avoid letting the drainage from vesicles fall down onto an unaffected eye as that can cause involvement