Lara Silverman MD/MPH, Emergency Medicine PGY3
Dizziness is vague, subjective, and the differential is literally everything from “you’re drunk go home” to life-threatening. Classically, we’re taught that dizziness is separated into 4 categories: vertigo (“room-spinning”), presyncope (“lightheadedness”), disequilibrium (“I feel unbalanced”), and non-specific / other. However, placing a patient in one of these categories relies on a patient’s subjective description of dizziness, which is notoriously variable, even within the same interview1 — not to mention unbelievably difficult over a translator phone. So why do we keep trying to place patients in these boxes, often dangerously anchoring on a diagnostic category that we came to through subjective data? Recently, there’s been lots of research that supports approaching dizziness differently, in a way that emphasizes timing, triggers, and additional symptoms.
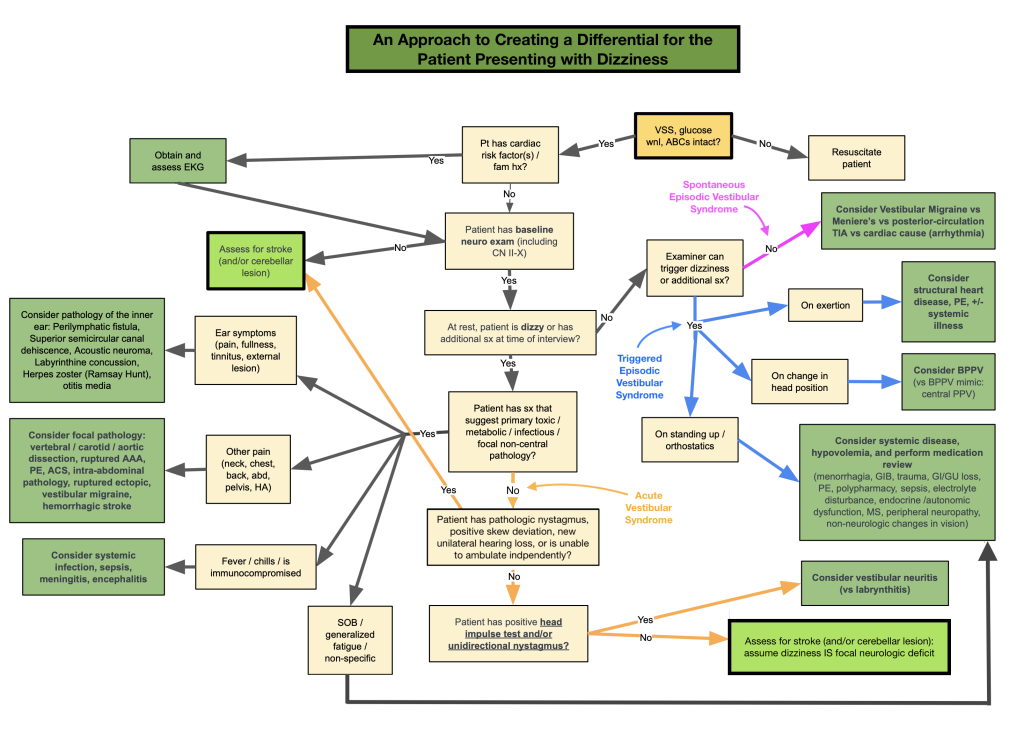
Specifically, much of the recent literature separates dizziness into three general categories: Acute Vestibular Syndrome (AVS, which refers to a patient with constant dizziness, most concerning for a stroke) and Episodic Vestibular Syndrome (EVS, which refers to dizziness that comes and goes), which is then sub-categorized as spontaneous or triggered. The basic diagnostic algorithm looks like this:
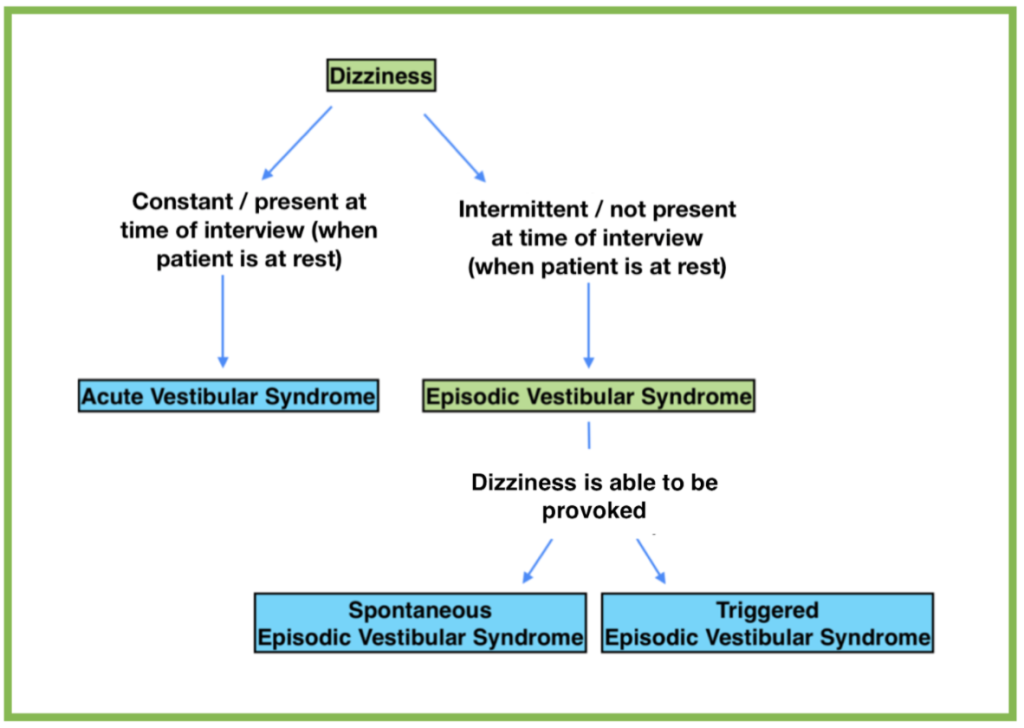
However, it is important to note that 50% of people who present with the chief complaint of dizziness actually have underlying metabolic derangements, toxicologic pathology, or infectious causes of dizziness,2 and this algorithm does not consider these. So first, I’ll walk through some basics of what causes dizziness, then I’ll attempt to incorporate some of the more broad differential diagnoses into the algorithm above.
The basics: Causes of Dizziness
I think of four general functional categories of dizziness: cardiovascular (dysrhythmias and valves), systemic derangements, neurological (the brainstem and cerebellum), and peripheral proprioceptive (the ear, vision, and MSK).
Cardiovascular:
The cardiovascular system is responsible for perfusing the brain. If there is cardiovascular pathology from dysrhythmia or structural heart problems, this can result in global brain hypoperfusion (interestingly, the retina is one of the first areas to be underperfused, resulting in the sensation of “blacking out!”). This includes hypoperfusion of structures like the cerebrum, homunculus, cerebellum, brainstem, and vestibulocochlear systems. Because of this, dizziness from cardiovascular causes can be described in many different ways, some sounding very similar to dizziness from vestibular or cerebellar causes.
In general, cardiovascular causes of dizziness tend to be acute in onset, associated with exertional triggers (structural abnormalities) or no triggers (dysrhythmias), and associated with cardiovascular risk factors or family history.
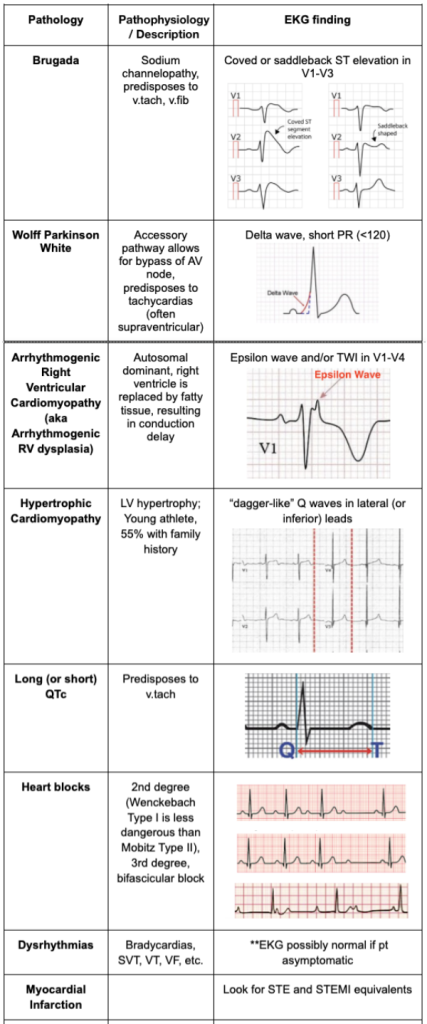
This type of dizziness is often on the spectrum with syncope and presyncope, and some studies have reported that up to 40% of “dizziness” in adults >65 were found to have an underlying cardiac cause.3 Have an extremely low threshold to get an EKG and if the symptoms are at all suspicious for structural abnormality (ie, associated with exertion), consider doing a cardiac POCUS to look for wall motion abnormalities, reduced cardiac output, right heart strain, gross valvular disease etc. If, after thorough evaluation, a patient is at high risk for underlying cardiac disease and there has been no other cause identified, these patients could be candidates for obs as a pre-syncope picture, or for referral to outpatient cardiology for holter monitor etc. The differentials in this category include:
- Dysrhythmias
- Bradycardia Tachycardia / Blocks (2nd degree, 3d degree, bifascicular)
- Brugada
- Wolff Parkinson White
- Arrhythmogenic right ventricular cardiomyopathy
- Structural heart problems
- Aortic / mitral stenosis
- Hypertrophic cardiomyopathy
- MI
- Heart failure
Systemic Derangements:
“Systemic Derangements” is broad and I find it to be one of the reasons dizziness is such a frustrating chief complaint. A third to half of all patients fall into this category,4 and it is extremely difficult for patients to describe these symptoms. Many of these underlying medical complaints will cause dizziness due to global hypoperfusion, similar to cardiac causes, however, the onset of this dizziness tends to be more insidious and symptoms generally are persistent rather than episodic.
Many of these diagnoses will reveal themselves in the vitals, labs, or with associated symptoms. Evaluate carefully for concurrent symptoms apart from neurologic complaints (ie, pain, diarrhea). If anything about a patient’s story or vitals doesn’t fit perfectly into one of the three “Vestibular Syndrome” categories (Acute, Spontaneous Episodic, or Triggered Episodic), consider sending at least a minimal workup.
The differential is huge and includes:
- Hypovolemia
- Acute blood loss anemia (ruptured ectopic, GIB)
- Dehydration, GI/GU loss
- Aortic dissection
- Ruptured AAA
- Medication side effects or overdose
- Ca channel / beta blockers, Antihypertensives
- Sepsis
- Anaphylaxis
- Electrolyte disturbance
- Endocrine abnormalities
- Autonomic dysfunction
- Hypo/erglycemia
- Pulmonary Embolism (S1Q3T3)
- Neurological abnormality (Diabetic neuropathy / Peripheral vascular disease)
- Wernicke’s encephalopathy / B12 deficiency
The Brainstem and Cerebellum:
These next two categories (brainstem / cerebellum and peripheral proprioceptive) are typically thought of when evaluating a patient for “dizziness” and account for most of the diagnoses in the “Vestibular Syndrome” framework noted initially. They can both be associated with nausea, vomiting, and gait instability.
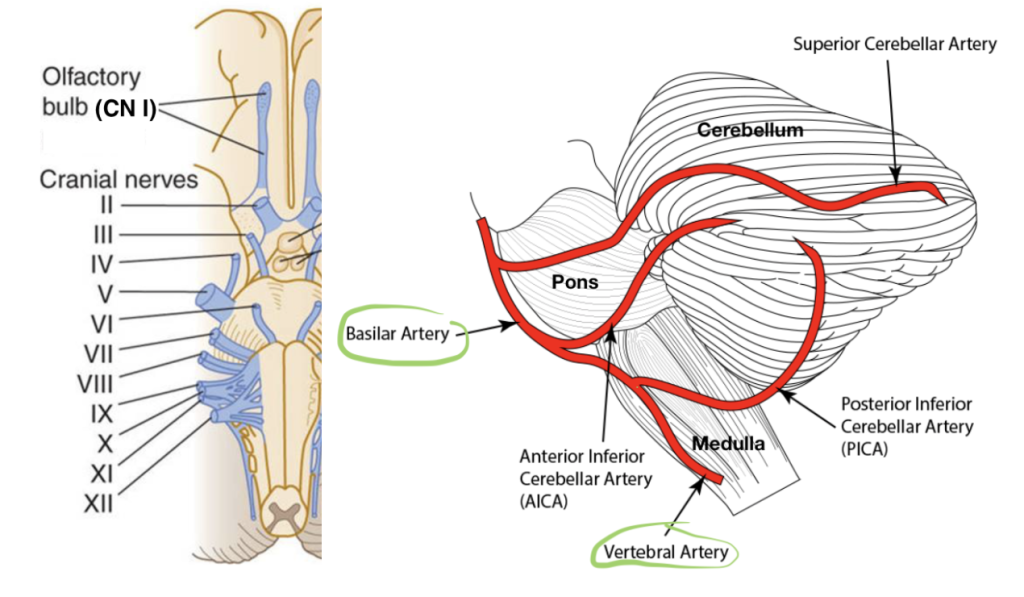
Centrally, the cerebellum is responsible for coordination, balance, and movement. The brainstem consists of the pons, which controls functions such as hearing, facial movements, and balance and the medulla oblongata which controls vital functions like breathing and heart rate. Remember that the cranial nerves also originate from the brainstem and cerebellum (10 of the 12 nerves originate in the brainstem; CN I olfactory and CN II optic originate in the cerebellum), which is important to consider when performing a physical exam.
The blood supply to the cerebellum and brainstem is from the posterior circulation, namely the vertebral and basilar arteries. Disruption of this blood supply is likely to cause insult to some combination of the cerebellum, brainstem, and cranial nerves, meaning that a patient will have dizziness plus some other focal finding. However, studies have shown that almost 25% of strokes involving the posterior circulation were isolated cerebellar strokes involving no other deficit,5 which poses diagnostic challenges when trying to differentiate between stroke and peripheral causes of dizziness.
As a generalization, pathology in this category tends to be associated with some other focal neurologic deficit (the “dizziness and” approach). However, as mentioned, this is only true in about 75% of posterior circulation strokes, meaning that 25% will only be caught with a nuanced physical exam (enter the HINTS exam… wait for it) or advanced imaging.
Additionally, these symptoms are commonly acute onset, persistent rather than episodic, and with no specific triggers. There is of course some nuance to this as structural lesions could be more gradual in onset and a transient ischemic attack is by definition transient and thus not sustained. A patient with a posterior circulation stroke will also likely feel worse with head movement, though they will usually have at least mild continuation of symptoms at rest and/or significant gait instability with true inability to walk independently.
Given the potentially deadly nature of diagnoses in this category, it is also important to risk-stratify individuals. Studies have shown that individuals who present with vertigo and 1-2 stroke risk factors have an 8% two-year stroke risk, and individuals with more than three risk factors have a 14% two-year stroke risk.6
Ischemia is a big can’t-miss diagnosis however, don’t overlook things like vertebral artery dissection, abscesses, or structural disease. Diagnoses in this category include:
- Posterior stroke / TIA
- Vertebral artery dissection
- Cerebellar abscess / mass
- Migraine
- Multiple Sclerosis
- Acute alcohol intoxication
- Cerebellar toxicity from chronic alcohol use
The Ear, Vision, & MSK system (Peripheral Proprioception):
The next category is one we often refer to as “peripheral” and can be extremely difficult to distinguish from central causes of dizziness. It is worth noting that the modern framework on dizziness uses “vestibular syndrome” to refer to the nature of symptoms rather than the origin of the symptoms. Thus, “acute vestibular syndrome” could refer to dizziness caused by a central stroke. Here, however, we will discuss the vestibular apparatus, which includes the organs of the inner ear.
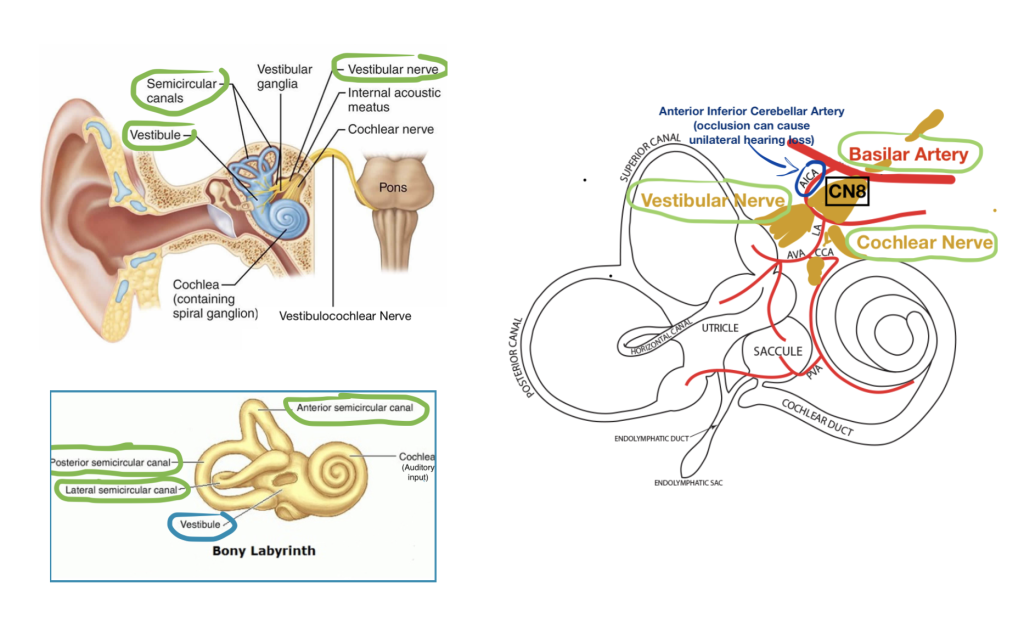
Specifically, there are three main components in the inner ear that can go awry and cause dizziness:
1. The Vestibule (composed of the otolith organs: utricle and saccule) contains tiny ear rocks (otoconia), which move in response to gravity, helping to distinguish whether you’re up or down.
2. The Semicircular Canals are fluid-filled organs with tiny hair cells that bend as you bend, helping the body interpret movement.
3. The Vestibular Nerve (which combines with the cochlear nerve to form CN 8, the vestibulocochlear nerve) takes information from the vestibule and semicircular canals and transmits it to the brain.
These vestibular structures also send signals directly to structures that control eye movements, which allows for reflexive coordination between eye movement and head movement.
It is important to note that vestibular input is transmitted separately from the cochlea’s auditory input and each system is supplied by a branch of the basilar artery. Historically hearing loss was thought of as a symptom of peripheral pathology, however thinking on this is changing given data that show an Anterior Inferior Cerebellar Artery (AICA) stroke (ie, a stroke in the vessel that supplies CN8 at the junction of the vestibular and cochlear nerves), was responsible for nearly half of all dizziness cases that were appropriately evaluated but falsely attributed to a peripheral non-ischemic cause7.
Apart from the structures of the inner ear, the brain receives information about where the body is in space from the musculoskeletal system and the visual system. A person could also experience dizziness if either of these systems are not appropriately sending signals to the brain, due for example to peripheral neuropathy in the setting of diabetes.
Diagnoses in this category are typically thought of as positional and episodic, lasting seconds to hours. The positional and episodic nature comes from the brain not being able to interpret the awry vestibular signals when the head moves, causing dizziness. At rest, the vestibular apparatus is not attempting to communicate information about position change and patients are typically asymptomatic. Patients are often reluctant but able to walk. Additionally, though nausea and vomiting can be associated with both central and peripheral lesions, severe symptoms are more commonly associated with peripheral lesions than with central lesions.8 Paroxysmal Positional Vertigo (BPPV) and Meniere’s Disease are the two most common causes of peripheral vertigo,9 however, it is important to note that there are many other diagnoses in this category such as structural abnormalities and infectious syndromes which will be more subtle and persistent in nature. The majority of these less prominent diagnoses are associated with other physical symptoms or exam findings involving the ear (pain, fullness, lesions, etc; not including hearing loss). Common diagnoses include:
- Benign Paroxysmal Positional Vertigo (most common)
- Meniere’s Disease (2nd most common)
- Persistent pathology of the structures of the ear vestibular system:
- Perilymphatic fistula
- Superior semicircular canal dehiscence
- Acoustic neuroma
- Labyrinthine concussion
- Infectious / inflammatory process of the inner ear:
- Herpes zoster oticus
- Vestibular neuritis (3rd most common)
- Labyrinthitis
- Otitis media
- Other peripheral proprioceptive abnormality:
- Change in vision
- Disorder of peripheral nerves (peripheral neuropathy)
- MSK disorder Drug ototoxicity
The HINTS Exam: Stroke vs Vestibular Neuritis
For persistently dizzy patients (+/- unsteady gait and nystagmus)
One of the first diagnostic questions to consider in a patient with dizziness is stroke vs no stroke. If symptoms are episodic, reproducible, and the patient is completely asymptomatic at the time of interview (including normal neurological exam and independent steady gait), the cause is highly unlikely to be central. If a patient has persistent or spontaneously episodic symptoms (ie, episodes not triggered by anything including position), look for other new focal neurological deficits. If found, proceed with stroke protocol.
As discussed, however, a quarter of all posterior circulation strokes present as isolated dizziness and have no other associated symptoms or neurological deficits. Vestibular neuritis (inflammation of the vestibular nerve) is a benign syndrome lasting only a few days that presents in a very similar way to stroke and is diagnosed in roughly 10% of patients presenting with dizziness.11 It presents reasonably acutely (often after a viral illness) and is associated with persistent isolated dizziness. So how do we distinguish isolated cerebellar stroke from vestibular neuritis? There are key differences that a skilled clinician can elucidate on physical exam, and distinguishing between these two specific diagnoses (posterior circulation stroke presenting with isolated dizziness and vestibular neuritis) is the purpose of the HINTS exam.
Emergency physicians use this test incorrectly more than 93% of the time, giving it extremely low diagnostic value.12 However, with proper training, the sensitivity and specificity of the exam performed by ED docs rivals those of neuro-ophthalmologists, >96%(!).13,14
The basic question the HINTS exam is trying to answer is: Is this patient’s dizziness a focal neurological deficit for which I should be pursuing a stroke work up? Thus, the HINTS exam should only be performed on a specific patient population with isolated rapid-onset dizziness that is constant and ongoing.15 (Notably, peripheral pathology will cause unidirectional nystagmus, and there are conflicting opinions about whether or not nystagmus must be present in order for the HINTS exam to yield meaningful results. For our purposes, we will assume the only required prerequisite is that the patient have persistent dizziness.) There are three components to the traditional HINTS exam: the Head Impulse test, the test for Nystagmus, and the Test for Skew. SAEM has proposed that we begin to perform a “HINTS plus” exam, which includes a finger rub hearing test given the association between AICA strokes and new-onset unilateral hearing loss.16 A stroke workup should be pursued if there are any pathologic findings, or if the patient has no signs of peripheral pathology to explain the dizziness (assuming all other causes of dizziness–systemic, infectious, metabolic, tox, psych, etc– have been ruled out).
The Head Impulse Test:
Is the Vestibulo-Ocular Reflex (a peripheral reflex) Intact?
The head impulse test is testing a component of the Vestibulo-Ocular Reflex, a peripheral reflex that helps the eyes make extremely rapid micro-adjustments as the head moves so that we can, for example, read a street sign while we walk. It sends signals from the vestibular organs in the inner ear directly to the extraocular muscles of the eye via the vestibular nerve without requiring processing in the cerebellum, allowing it to make adjustments extremely fast, seemingly seamlessly.17
In a healthy individual, this reflex should allow eyes to smoothly track or remain fixated on objects as the head moves. However, if the vestibular neuron is inflamed and not sending signals appropriately, the eyes will require the slightly slower input from processing centers in the brainstem (specifically the vestibular nuclei) to track objects, resulting in a delayed “corrective saccade” to return back to a target.2
Importantly, this test only asks about the presence or absence of this peripheral reflex, and will not tell you anything specific about whether or not there is a central lesion. Do not use this test to “rule in” a central lesion.
How to perform the head impulse test:
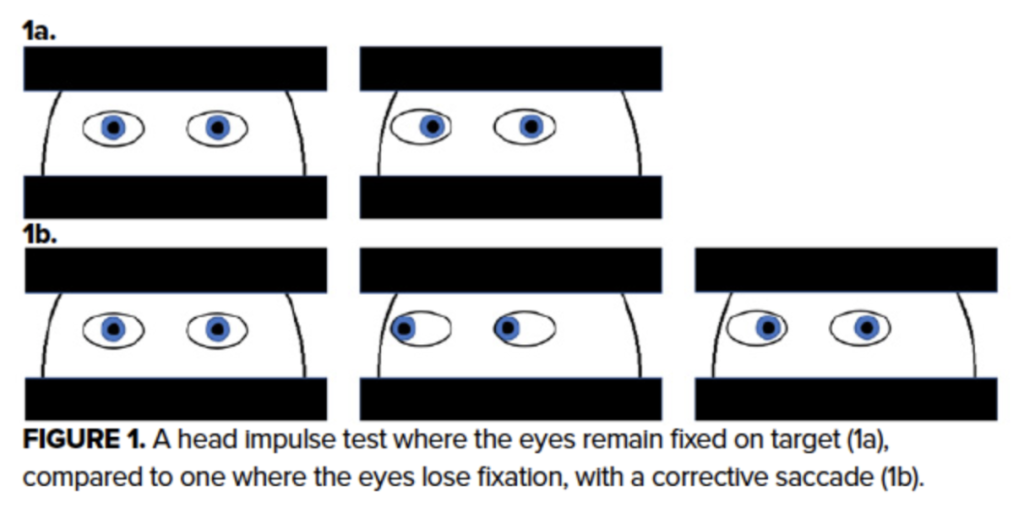
Corrective Saccade = Peripheral Lesion
Smooth Tracking = No Peripheral Lesion
- Tell a patient to focus on a distant target (or the examiner’s nose)
- Hold the patient’s mandible (Alternatively, you can help the patient loosen up by moving their face slowly in multiple directions while they focus on your nose)
- Without warning, turn the patient’s head suddenly 15 degrees in any direction
- Observe whether the eyes stayed smoothly fixed on the target (normal vestibulo-ocular reflex), or required a corrective saccade (abnormal reflex, likely vestibular neuritis or rarely other lesion in the vestibular system).
Evaluating for Nystagmus: Is there evidence of a central lesion?
When a person moves their eyes laterally in one direction, ligaments exert an elastic force on the eye in an effort to keep the eye in neutral position. In order to allow the eye to move laterally, a network involving the cerebellum (called the neural integrator) signals a fast corrective contraction, pulling the eye in the intended direction. Normally, this corrective contraction is undetectable, however even in a healthy person, we might see mild nystagmus with far lateral movement.18,19
Nystagmus has two phases: the slow pull of the elastic ligaments and the fast corrective pull from the in the opposite direction. Peripheral pathology will cause notable unidirectional nystagmus, in which either nystagmus only occurs when looking one direction, or if nystagmus occurs in both directions, the fast phase is always opposite the side with the lesion.18 For example, if the lesion is on the right, the faster phase will be to the left when looking left and to the left when looking right–think of this as the right side not being able to send “fast” signals because it has pathology. Because the cerebellum is still able to process and ultimately quiet these incorrect signals, nystagmus caused by peripheral lesion tends to be fatiguable and less pronounced.
In central pathology, however, the neural integrator is unable to send messages appropriately in either direction, and the push-and-pull between the ligamentous elastic force and the corrective contraction is pronounced, prolonged, and bidirectional.20 In bidirectional nystagmus, the faster phase is always lateral or always medial (ie, it changes direction from left to right depending on the direction the patient looks). Note that the HINTS exam evaluates horizontal gaze-evoked nystagmus specifically, but any vertical or rotational nystagmus (which occurs via a different mechanism) is always pathologic.21
How to perform a test for nystagmus:
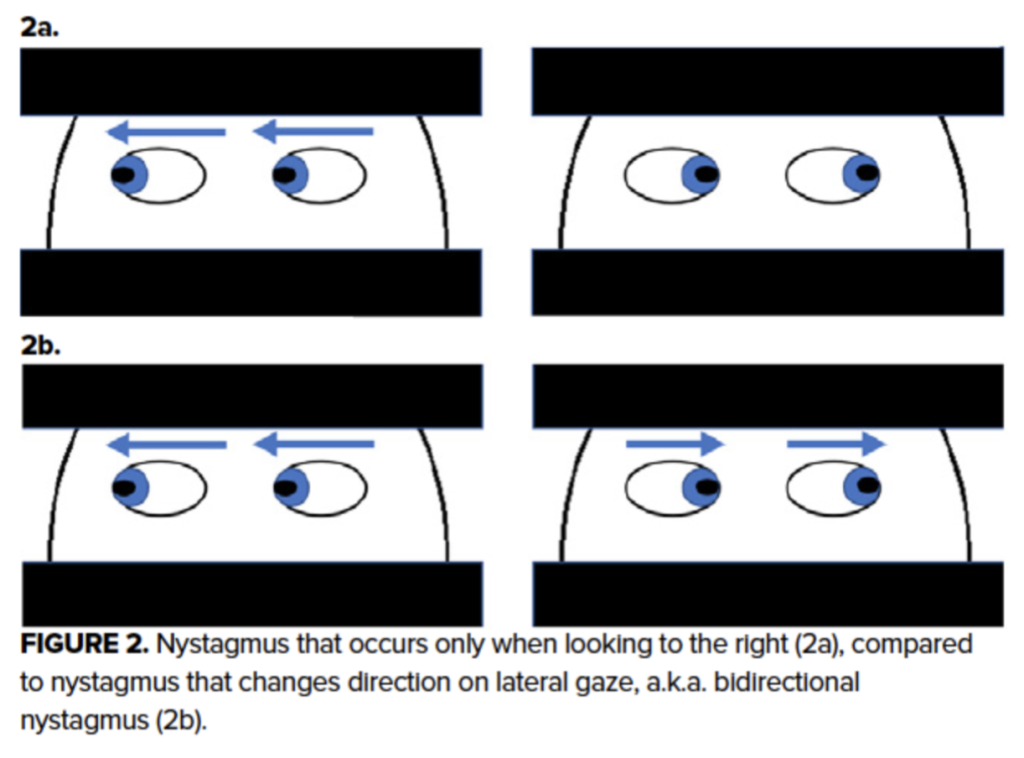
Bidirectional, vertical, or torsional nystagmus = Central lesion
Unidirectional nystagus = Peripheral lesion
No or physiologic nystagmus = No evidence of peripheral lesion, cannot rule out central lesion
- Tell a patient to look straight ahead. Evaluate for any nystagmus at rest.
- Tell a patient to follow your finger as you move it 20 degrees to the right. Evaluate for nystagmus. Note whether the beat of the nystagmus is faster when the eye is being pulled laterally or medially.
- Have the patient follow your finger back to center and then 20 degrees to the left. Evaluate for nystagmus. Note whether the beat of the nystagmus is faster when the eye is being pulled laterally or medially.
Testing for Skew: Is there evidence of a central lesion?
The test of skew also evaluates for the presence of a central lesion. Skew deviation results from dysfunctional afferent signals (from the brain to the eye) in a pathway that uses gravity to orient the eye known as the Graviceptive Pathway. The Graviceptive Pathway involves input from the inner ear to inform the brain of the head’s relationship to gravity. The brain interprets this input, and sends signals to the ocular muscles. If the head tilts, this pathway makes adjustments to reorient the eyes and if the head is stationary, those signals are conveyed as well.
When the central processing malfunctions (ie, in the setting of stroke or central lesion), pathways that align the eyes using gravitational input do not interpret or send information appropriately. Thus, when gravitational input alone is used to orient the eye, the eye becomes misaligned.22 Though the exact mechanism is not clear, covering one eye results in vertical misalignment and restoring visual input corrects this.
How to Test for Skew
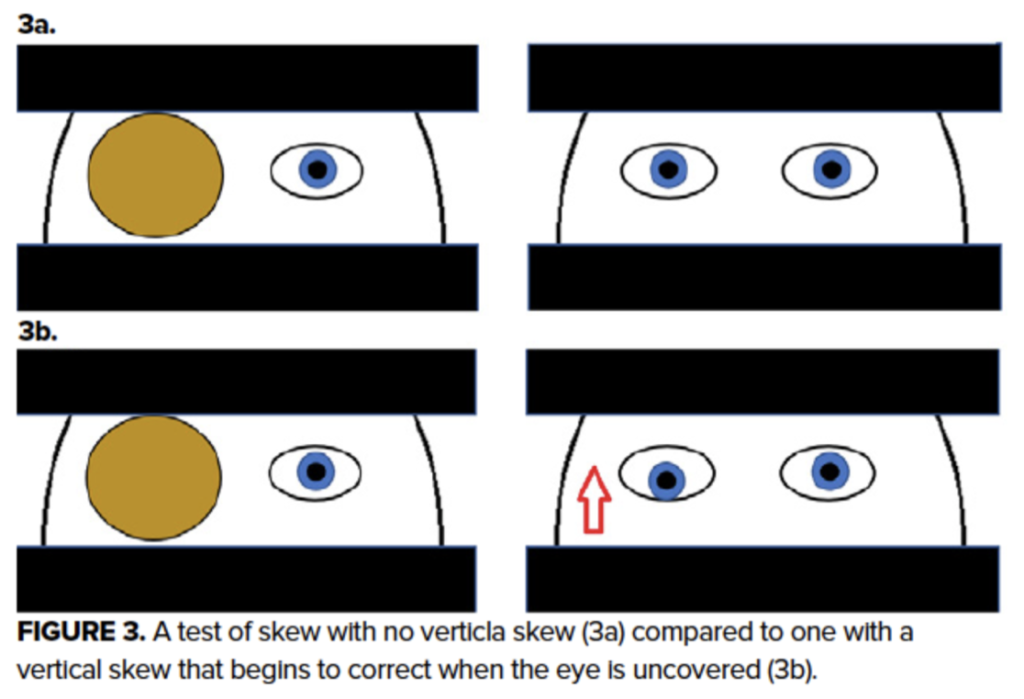
Vertical Misalignment = Central Lesion
No Vertical Misalignment = No definitive evidence of central lesion
- Cover one eye completely for several seconds
- Quickly remove your hand
- Observe for realignment of the covered eye
- Repeat with the other eye
HINTS Plus: Adding a Hearing Friction Rub Test
The HINTS exam is able to test for peripheral pathology by looking for unidirectional nystagmus and by looking for a corrective saccade on the Head Impulse Test. The HINTS exam tests for central pathology by looking for pathologic central nystagmus and skew deviation. However, if there is an infarct in the Anterior Inferior Cerebellar Artery (AICA), which supplies CN8 (the vesibulocochlear nerve) this could present clinically as a peripheral lesion, while actually being caused by more concerning ischemic pathology. For this reason, SAEM is in the process of devising recommendations to include a friction rub test to look for new unilateral hearing loss, which would be likely in the case of an AICA infarct, but not in the case of an isolated vestibular neuritis.
TL;DR: Summary
Whew, that was a lot. If you made it this far, I’m impressed. In brief, here’s what we learned:
- Instead of the “how did they describe their dizziness” approach, focus on timing, triggers, and associated symptoms
- Literature is dividing dizziness into three general categories: Acute Vestibular Syndrome (AVS, constant dizziness, concerning for stroke)Spontaneous Episodic Vestibular Syndrome (S-EVS)Triggered Episodic Vestibular Syndrome (T-EVS)
- I think of 4 general functional categories of dizziness:
- Cardiovascular causes:
- Acute onset, episodic
- No trigger (arrhythmia) or exertional trigger (structural cause)
- On the syncope/presyncope spectrum
- Low threshold for EKG
- Systemic Derangements:
- More gradual onset, persistent
- Associated with vital or lab abnormalities
- Associated with other non-neurologic symptoms
- Symptoms often orthostatic in nature
- Brainstem and Cerebellum causes (“central”):
- Generally acute onset, persistent
- In general, no triggers
- 75% of strokes are associated with another focal neurologic deficit
- Risk stratify (14% 2-yr stroke risk if dizzy + 3 or more risk factors)
- Peripheral Proprioceptive causes (“peripheral):
- Acute onset, episodic (seconds to hours)
- Triggered by position
- The vestibular apparatus (inner ear) sends information to the brain about orientation in space and to the eye for reflexive movements
- Proprioceptive information also comes from the limbs and visual input
- The AICA supplies blood CN8 (CN8= vesibular + cochlear nerves)
- Prevalence: BPPV > Meniere’s > Vestibular neuritis
- Cardiovascular causes:
- The HINTS Exam:
- The purpose of the HINTS exam is VERY SPECIFIC: evaluate a patient who has persistent ongoing dizziness for stroke (scary) vs vestibular neuritis (benign, usually resolves within ~3 days)
- There are 3 components to the HINTS exam; SAEM suggests we add a 4th to test for new unilateral hearing loss
- Head Impulse Test: Tests for peripheral neuritis
- Move the head quickly 15-20 degrees off center and look for a “corrective saccade”
- A corrective saccade indicated that the vestibular nerve is likely inflamed: vestibular neuritis is likely
- DOES NOT give any information about the presence or absence of a peripheral lesion
- Test for Nystagmus: Tests for central and peripheral lesions
- Have the patient follow your finger 20 degrees off-center and look for the presence of gaze-evoked nystagmus
- Peripheral lesion: Unidirctional nystagmus, fatiguable
- Central lesion: Bidirectional, vertical, or rotational nystagmus
- Head Impulse Test: Tests for peripheral neuritis
- Test of Skew: Tests for central lesion
- Cover one of the patient’s eyes. Quickly uncover the eye and look for skew deviation
- Skew deviation in either eye indicates a central lesion
- Finger rub hearing test: Tests for new-onset unilateral hearing loss
- Can indicate a stroke in the Anterior Inferior Cerebellar Artery (supplies CN8, the vestibulocochlear nerve)
Other Stuff
An Algorithm
There are many algorithms for dizziness out there and most of them address only patients who we already believe fall into one of the three vestibular syndrome categories. However, teasing out stroke vs some serious underlying systemic toxic, metabolic, infectious, or cardiac cause is one of my biggest concerns. After looking at many algorithms, I have come to the conclusion that we have two big obligations: 1) to thoroughly consider, assess for, and rule out stroke to the best of our abilities and 2) to consider the “everything else” category. Unfortunately, there is a huge amount of clinical context and judgement that needs to come into play and the bottom line is that there is no perfect algorithm. Nonetheless, this is an adaptation of an algorithm from a 2016 paper that I thought did a good job of trying to organize the various differential diagnoses. Note that this algorithm uses the pieces of the HINTS exam, but not in the HI-N-TS order. As always, this is a tool to help organize thinking, and should never take the place of critical thinking, a good physical exam, or clinical judgement.
Dot Phrases
As always, use dot phrases as guidelines to help you organize efficient and accurate documentation. Never document a part of a physical exam you did not perform. This is a dot phrase for an ABNORMAL HINTS exam as would be expected in a person with peripheral vestibular neuritis or labrynthitis.
.HINTS (POSITIVE for PERIPHERAL LESION; to be entered in HENT click box):
No bidirectional, horizontal, or rotational nystagmus. No nystagmus in neutral position. (***+/-Unidirectional nystagmus.) No skew deviation or vertical corrective movement in either pupil when independently covered and uncovered. Eyes with +corrective saccade when head is spontaneously moved rapidly 20 degrees off center in head impulse test.
Resources and References:
1: David E. Newman-Toker, Lisa M. Cannon, Matthew E. Stofferahn, Richard E. Rothman, Yu-Hsiang Hsieh, David S. Zee, Imprecision in Patient Reports of Dizziness Symptom Quality: A Cross-sectional Study Conducted in an Acute Care Setting, Mayo Clinic Proceedings, Volume 82, Issue 11, ISSN 0025-6196; https://doi.org/10.4065/82.11.1329.
(https://www.sciencedirect.com/science/article/pii/S0025619611614110)
2: Edlow JA. A New Approach to the Diagnosis of Acute Dizziness in Adult Patients. Emerg Med Clin North Am. 2016 Nov;34(4):717-742. doi: 10.1016/j.emc.2016.06.004. Epub 2016 Sep 7. PMID: 27741985.
3: Maarsingh OR, Dros J, Schellevis FG, van Weert HC, van der Windt DA, ter Riet G, van der Horst HE, Causes of persistent dizziness in elderly patients in primary care. Fam Med. 2010;8(3):196.
4: Hain, Epidemiology of Dizziness. 2022, May. https://dizziness-and-balance.com/disorders/dizzy_epi.html
5: Baier B, Conrad J, Stephan T, Kirsch V, Vogt T, Wilting J, Müller-Forell W, Dieterich M. Vestibular thalamus: Two distinct graviceptive pathways. Neurology. 2016 Jan 12;86(2):134-40. doi: 10.1212/WNL.0000000000002238. Epub 2015 Dec 11. PMID: 26659130
6: Lee CC, Su YC, Ho HC, Hung SK, Lee MS, Chou P, Huang YS. Risk of stroke in patients hospitalized for isolated vertigo: a four-year follow-up study. Stroke. 2011 Jan;42(1):48-52. doi: 10.1161/STROKEAHA.110.597070. Epub 2010 Dec 2. PMID: 21127296.
7: Newman-Toker DE, Kerber KA, Hsieh YH, Pula JH, Omron R, Saber Tehrani AS, et al. HINTS outperforms ABCD2 to screen for stroke in acute continuous vertigo and dizziness. Acad Emerg Med. 2013;20(10):986-96.
8: https://www.emrap.org/episode/c3dizziness/c3dizziness
9: Smith T, Rider J, Cen S, et al. Vestibular Neuronitis. [Updated 2022 Jul 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549866/
11: Cutfield NJ, Seemungal BM, Millington H, et alDiagnosis of acute vertigo in the emergency departmentEmergency Medicine Journal 2011;28:538-539.
12: A Regis, B Oluwadamilola, R Lepage, Z Turgeon, S McIsaac, R Ohle, CDmitriew; Diagnostic Accuracy of the HINTS Exam in an Emergency Department: A Retrospective Chart Review doi: 10.1111/acem.14171; 2020 by the Society for Academic Emergency Medicine
13: Gerlier C, Hoarau M, Fels A, Vitaux H, Mousset C, Farhat W, et al. Differentiating central from peripheral causes of acute vertigo in an emergency setting with the HINTS, STANDING, and ABCD2 tests: A diagnostic cohort study. Acad Emerg Med. 2021;28(12):1368-78.
14: Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009;40:3504–3510.
15: Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009 Nov;40(11):3504-10. doi: 10.1161/STROKEAHA.109.551234. Epub 2009 Sep 17. PMID: 19762709; PMCID: PMC4593511.
16: Guidelines for Reasonable and appropriate care in the emergency department 3 (GRACE-3): Acute dizziness in the emergency department; 2022, Society for Academic Emergency Medicine; https://www.saem.org/docs/default-source/saem-documents/grace/grace-3-draft-acute-dizziness-%28no-endnote%29.pdf?sfvrsn=8a6491e_2
17: Broussard DM, Heskin-Sweezie R, Titley HK; Motor Learning in the Vestibule-Ocular Reflex; Encyclopedia of Behavioral Neuroscience, 2010; http://www.sciencedirect.com/science/article/pii/9780080453965002463
18: Murali Chand Nallamothu; Nystagmus. https://www.youtube.com/watch?v=UPYqd31hhfE&t=105s
19: Stuart A, Eggenberger E, Galetta SL, Gold D, Rucker JC; Making Sense of Acquired Adult Nystagmus; American Academy of ophthalmology; EyeNet Magazine; Oct 2016
20: Abadi RV. Mechanisms underlying nystagmus. J R Soc Med. 2002 May;95(5):231-4. doi: 10.1177/014107680209500504. PMID: 11983762; PMCID: PMC1279674.
21: Sanchez, K. and Rowe, F.J. (2018), Role of neural integrators in oculomotor systems: a systematic narrative literature review. Acta Ophthalmol, 96: e111-e118. https://doi.org/10.1111/aos.13307
22: Gold, Daniel R. DO; Schubert, Michael C. PT, PhD. Ocular Misalignment in Dizzy Patients—Something’s A-Skew. Journal of Neurologic Physical Therapy: April 2019 – Volume 43 – Issue – p S27-S30 doi: 10.1097/NPT.0000000000000271
HINTS Photo credit: https://www.emra.org/emresident/article/hints-exam/
