2 weeks ago, I had a patient presenting with an upper GI bleed. Despite aggressive treatment, the patient was still hypotensive and actively bleeding. Unfortunately, the GI fellow was on home call and further than expected from the hospital, but after telling him, “I’m placing a Blakemore,” he hurried in. That was a lie, I didn’t actually place a Blakemore; but GI did come to scope the patient. But should I have? When do I do it? Why do I do it? How do I do it? Let’s answer those questions.
Who: Patients presenting with suspected variceal bleeding (either they have known varices or other evidence of decompensated cirrhosis)
What: This is a Sengstaken-Blakemore tube

It is a long flimsy catheter that has both a gastric and esophageal balloon for tamponade, and a fenestrated end for suctioning stomach contents.
When: If medical management (antibiotics, PPI, Octreotide, blood products, pressors) fails and GI is not immediately nearby to scope. The patient should be intubated prior to placing the Blakemore.
Where: …really?
Why: The majority of variceal bleeds occur around the gastro-esophageal (GE) junction and a minority in the distal esophagus. The primary function of a Blakemore is to apply pressure to the GE junction through the use of the gastric balloon. If tamponade at the GE junction is not sufficient, then the esophagus balloon can be inflated to attempt tamponading the distal esophagus as well.
How: For this procedure, you’ll need a Blakemore catheter, two three-way stopcocks + male-female luer lock caps, a 50ml-syringe with a luer lock ending, a 50ml-syringe with a catheter tip, kelly clamps, cufflator, OG tube, kerlix, and a liter bag of saline.
Setup: The Blakemore comes with three ports; the gastric balloon, the esophageal balloon, and a gastric aspiration port. Don’t worry, everything is labeled!
The gastric and the esophageal balloon ports come with two plugs that should be removed first and then replaced with three-way stop cocks. One end of the three-way stop cock should be capped and the other end can be used to inflate the balloons with a 50ml syringe with a luer lock like this:
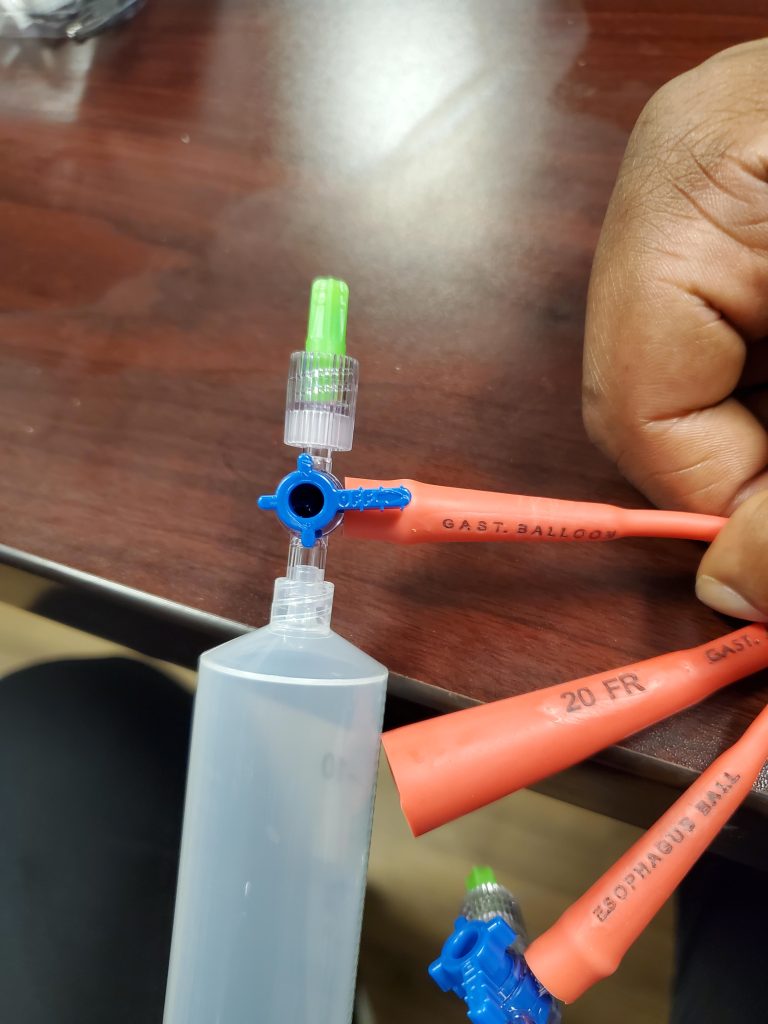
In Elmhurst, this works pretty well but I’ve noticed the three-way stopcocks sometimes leak air. In such a case, I would just use a 50ml syringe with a catheter tip and a kelly clamp.
Before beginning, check to make sure that both balloons properly inflate. Inflate them underwater to make sure that no air bubbles are leaking out.
Place the catheter and advance it about 50 cm to make sure that the gastric balloon is in the stomach (the last thing we need is for someone to try and inflate the gastric balloon in the esophagus).
Gastric balloon (Think Volume!): Inflate the balloon to about 50cc and then GET A PORTABLE X-RAY. After confirming that the gastric balloon is below the diaphragm, you can then inflate the gastric balloon to 250cc.Put the catheter under tension by tying the distal portion of the catheter to a saline bag (or any 1kg weight) and hanging it to gravity.
Esophageal balloon (Think Pressure!): If bleeding still isn’t controlled, the esophageal balloon can be inflated. Use a cufflator to inflate the esophageal balloon to30mmHg. Here is an EMRAP video of the entire process described above:
And if you don’t know, now you know
