More than just what company makes it
Written by Erena Weathers
Pacemakers have their own code.
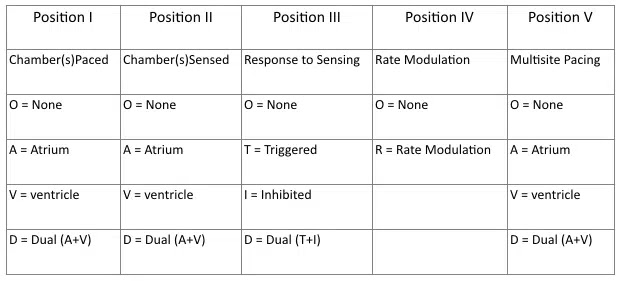
Position I: which chamber is paced
Position II: where the pacemaker senses the intrinsic rhythm
Position III: response to sensing
- T = Sensed activity results in triggering of paced activity
- I = Sensed activity results in inhibition of pacing activity
Position IV: rate modulation designed to the heart appropriately to meet certain physiological needs e.g. physical activity. Sensors may measure and respond to variables including vibration, respiration, or acid-base status.
Position V: indicates if multiple pacing areas in the chamber
Common Pacing Modes
AAI – Atrial pacing and sensing
- atrial paced and sensed, inhibited
- used in sinus node dysfunction with intact AV node
VVI – Ventricle pacing and sensing
- ventricle paced and sensed, inhibited
- Used in those with chronic atrial dysfunction such as afib/aflutter
DDD – dual dual dual
- atrial paced if no intrinsic rhythm and same for the ventricle for set time after atrial pacing
- atrial channel function is suspend during a fixed periods following atrial and ventricular activity to prevent sensing ventricular activity or retrograde p waves as native atrial activity
Magnet Mode
- activated by placing a magnet over the device, activates a special mode
- Usually an asynchronous mode which delivers a constant rate
- asynchronous mode ventricular pacing increases risk for ventricular tachycardia/dysrhythmia
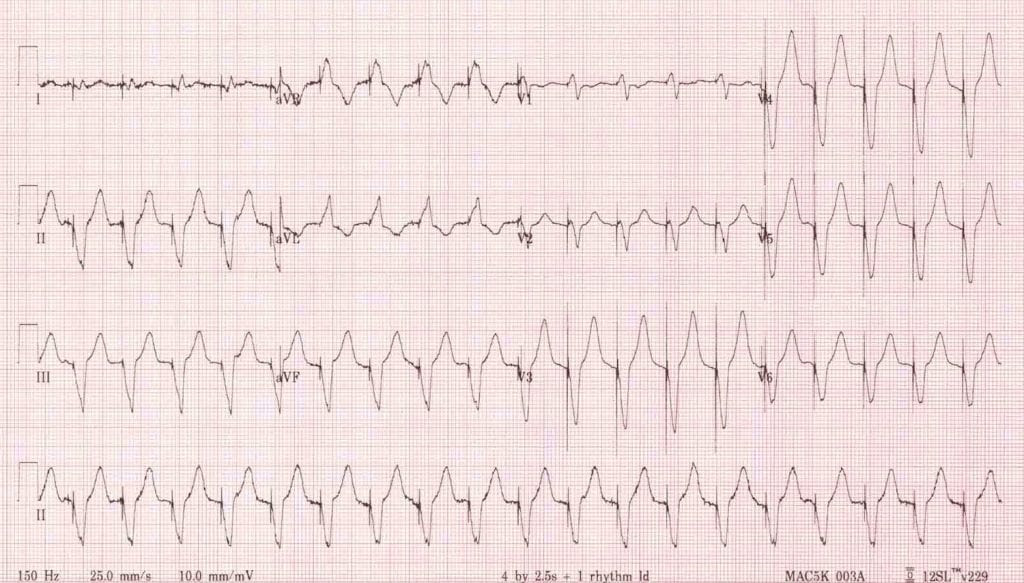
Paced EKGs
You can tell a person has a pacer because of spikes on the EKG. The spikes depend on the lead placement and may sometimes not be seen in all leads.
Atrial Pacing: spike precedes the p-wave
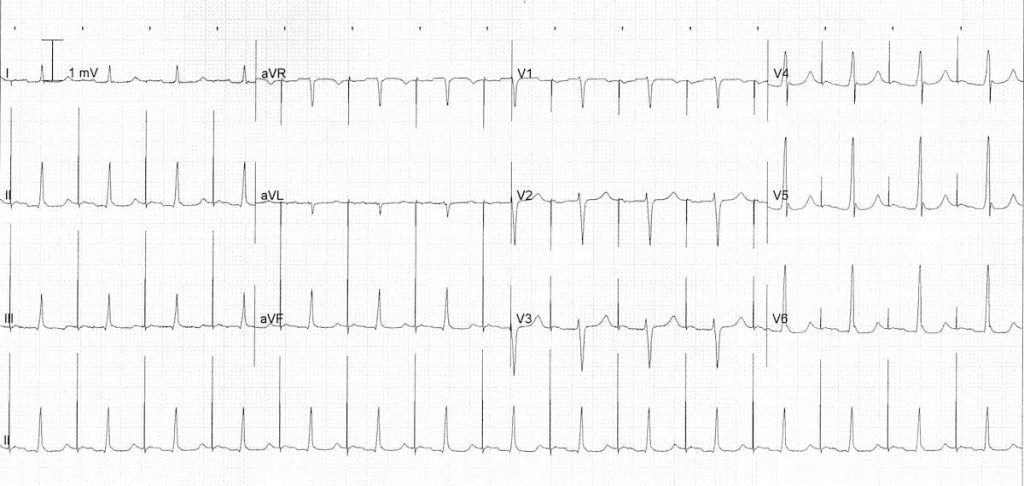
Ventricular Pacing: spike precedes the QRS complex. If the right ventricle is paced then a LBBB pattern is formed, and if the left ventricle is paced then a RBBB pattern is formed.
Dual Chamber: features of both atrial and ventricular pacing spikes, they can precede the p wave or the QRS or neither.
So now that we covered that, let’s look at what goes wrong.
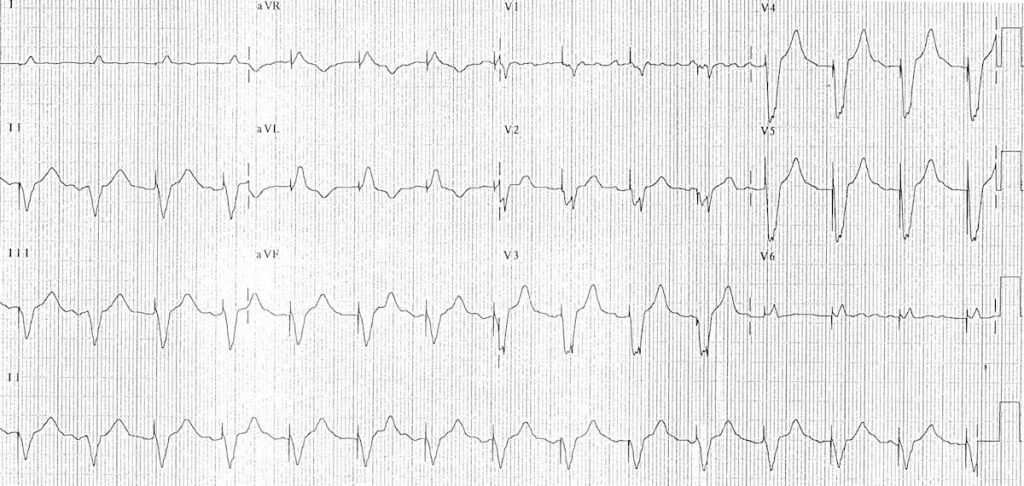
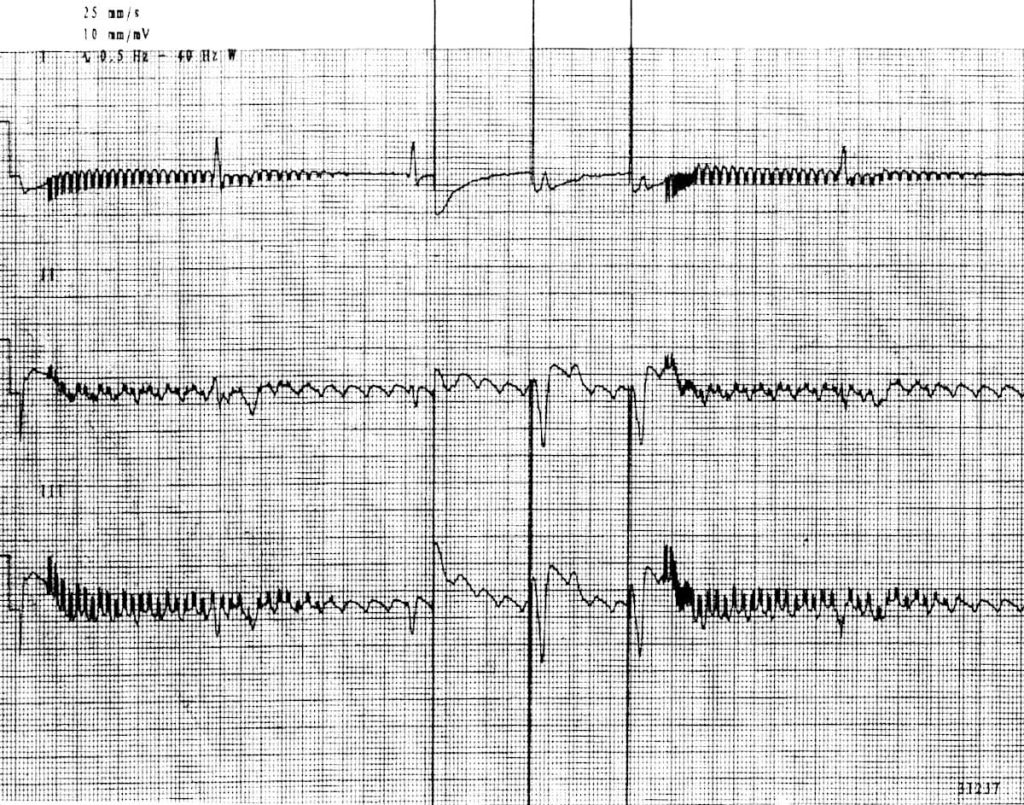
Sensing Problems
Undersensing: the pacemaker fails to sense the intrinsic rhythm leading to asynchronous pacing. This is due to an “exit block” in which the lead doesn’t depolarize the endocardium adequately. EKG findings include spikes earlier than the programmed rate, spikes within the QRS complex, no QRS after spike if in refractory period.
Oversensing: the pacemaker inappropriately reads other signals as an intrinsic rhythm eg. muscle twitches or chest wall movement. It may not be easily seen on EKG, but could be due to large P or T wave, could be due to ipsilateral cell phone use, and can be triggered if the patient activates his pectoralis muscles.
Pacing Problems
Output Failure: paced stimulus is not generated when expected. Could be due to oversensing, lead fracture, displacement, or interference.
Failure to Capture: paced stimulus does not result in myocardial depolarization, so you won’t see a QRS complex. Could be due to electrode displacement, wire fracture, electrolyte disturbance, MI, or exit block.
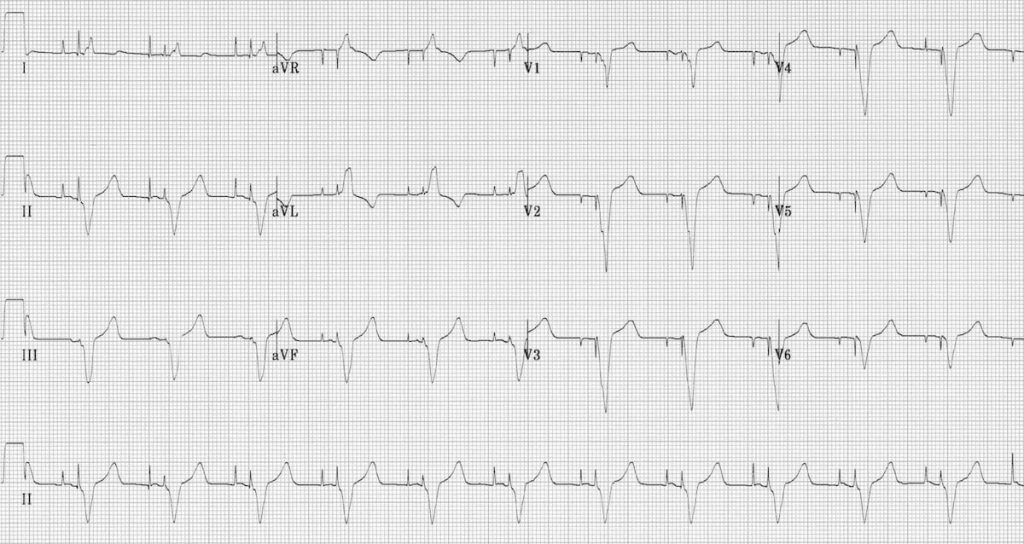
Pacemaker Dysrhythmias
Lead Displacement Dysrhythmia: pacing wire is floating around the chamber, and intermittently touches the ventricular wall causing ventricular ectopics or runs of VT with episodes of failure to capture. You will see changes in the QRS complex on the EKG and will see the wire on CXR.
Pacemaker Mediated Tachycardia: This is a re-entry tachycardia where the pacemaker forms the antegrade pathway with retrograde conduction by way of the AV node. Retrograde p waves are read as intrinsic rhythm and then ventricular pacing starts, the tachycardia is maxed at the programming of the pacemaker. To treat you give an AV nodal blocker and/or place a magnet to switch to asynchronous mode.
Sensor Induced Tachycardia: This is due to a pacemaker being set to increase the rate to certain stressors (ie physical activity) but now is increasing rate inappropriately. This could be due to vibrations, loud music, muscle twitches, or even electrical cautery in surgery. The ventricular rate cannot exceed the max rate set by the pacemaker. You place a magnet to terminate this.
Runaway Pacemaker: this is seen in older models in which there is a low battery and there is inappropriate excessive firing of the leads to >200 bpm. You can see very high ventricular rates which predispose to dangerous ventricular dysrhythmias. You can also have bradycardia since the ventricle is being overstimulated and unable to depolarize properly and/or the spikes are so small due to the low battery you have failure to capture.
Pacemaker Syndrome: This is when there is improper timing between the atrial pacing and ventricular pacing. The patient will have symptoms of shortness of breath, dizziness, weakness. You test for this by seeing a >20mmHg drop in BP when switching between paced and natural rhythms.
Twiddler’s Syndrome: This is caused by the patient somehow manipulating the pulse generator (the part in the pouch on the chest) causing it to twist on its vertical axis. This causes lead displacement and can have weird outcomes like diaphragm and arm twitching.
References
Burns E, Buttner E. “Pacemaker Malfunction.” Life in the Fast Lane. 4 Jun 2021. https://litfl.com/pacemaker-malfunction-ecg-library/
Swaminathan, Anand. “Pacemaker Basics.” REBEL EM. 24 Aug 2017. https://rebelem.com/pacemaker-basics/
