If you’re like me, when you treat hyperkalemia, you make things easy on yourself and open up that HyperK orderset, or think about the mnemonic C BIG K DROP (Calcium, beta-agonist/bicarb, insulin, glucose, Kayexalate (Lokelma actually), Diuretics, ROP (“renal unit for dialysis of patient”). Then you move on with your life, recheck the BMP and decide if you need another round, or you have to bring out the big guns with dialysis.
But if you’re like me, you may have been doing something wrong! Why is this?
Well, to summarize Josh Farkas, there are three proposed mechanisms for how bicarb should work for decreasing potassium. 1) Transcellular shift of K into muscle cells via alkalinization of serum or a HCO3/K cotransporter 2) renal excretion of K, which is upregulated with alkalinization and 3) dilution – by expanding extracellular fluid with isotonic bicarb, you dilute the concentration of K.
The PROBLEM with the order set we use is that it’s an ampule of 8.4% of Sodium bicarbonate when in reality, we should be giving ISOTONIC bicarb to these patients. The reason for this is that hypertonic fluids actually INCREASE serum potassium via solute drag. Studies on 8.4% bicarb show no effect on potassium, but 4.2% (used in Europe) or isotonic 1.3% show better results.
Furthermore, even isotonic bicarb seems to be ineffective in patients without a concomitant metabolic acidosis. For these reasons and more, the right patient to select bicarb for would be the one who is volume depleted, hyperkalemic, and with a metabolic acidosis, because an isotonic bicarb drip would solve all of these problems at once. To make this drip, you need 3 amps of bicarb in 1L D5W.
In an effort not to make this pearl go on forever. I’ll leave you with a couple more tidbits on bicarb, and two links to what I find very compelling reading from Farkas.
Isotonic bicarb should be in our fluid algorithm strategy, and it’s summarized as follows.
Isotonic bicarb: for volume deplete patients with NAGMA OR AGMA with uremia
Normal saline: for volume deplete patients with a PRIMARY metabolic alkalosis (think contraction alkalosis especially)
Lactated ringers or plamalyte: for volume deplete patients without any pH disorder
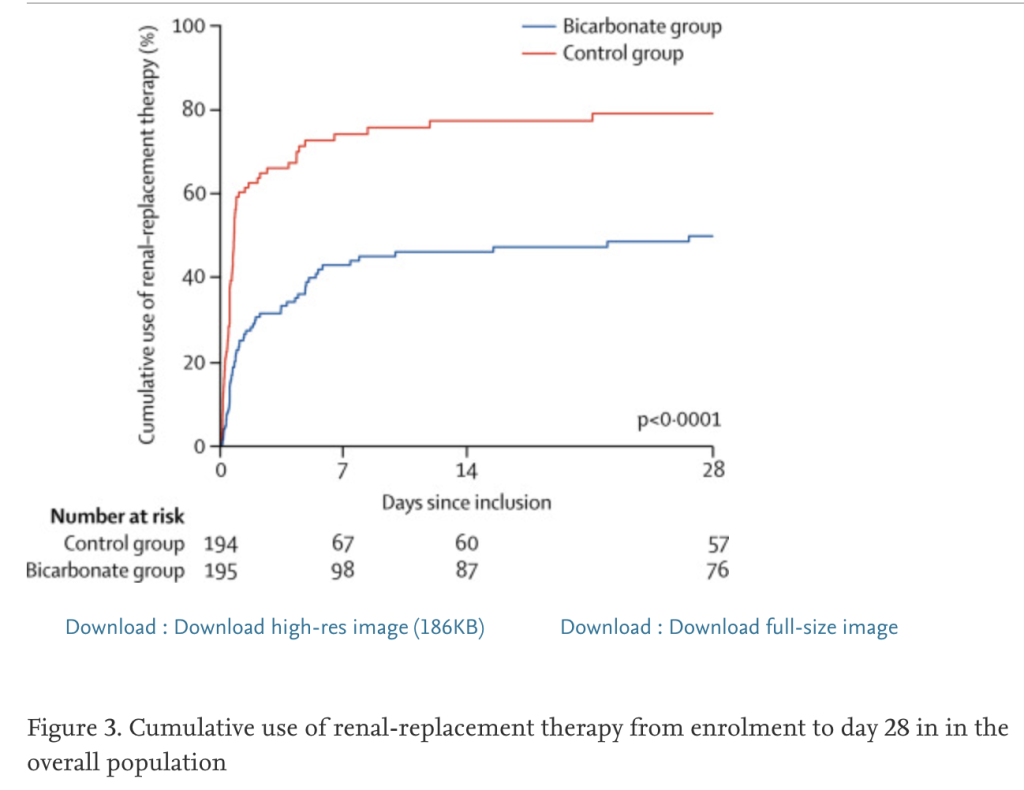
The BICAR-ICU trial (discussed heavily in the readings above), showed a mortality benefit in ICU patients with metabolic acidosis who received isotonic bicarb ONLY for those patients with a concomitant AKI. However, the secondary endpoint showed a statistically significant decrease in dialysis initiation. That’s a big deal.
And last tidbit: what about that acidotic patient you’re about to intubate? Again, anecdotally, I push bicarb right before intubation (IF I can ventilate them with bipap or bag them because otherwise it will convert to CO2 and become counterproductive). But again, there’s no data to show this is beneficial. Here’s part of a rebelEM review about resuscitating before intubation that highlights that lack of evidence, but also explains how to use the bipap machine to assist you).
