Causes
- Inadvertent intravascular injection (even without exceeding max dose)
- Overdose (with single or multiple doses)
- Absorption from a vascular area
Prevention
- Calculate max dose, considering comorbidities
- Direct US guidance, use saline to improve needle tip visualization
- Add epinephrine when possible. Epi decreases the systemic absorption of LA by reducing local blood flow, also if inadvertently injected IV will provoke tachycardia that can be seen on the monitor.
Presentation
| CNS symptoms | Cardiovascular symptoms |
| Tongue and perioral numbness | Hypertension and tachycardia |
| Paresthesias | Vasodilation and hypotension |
| Restlessness | Bradycardia, AV blocks |
| Tinnitus | Prolonged PR and QRS |
| Fasciculations or tremors | Ventricular arrhythmias |
| Tonic-clonic seizures | Refractory shock |
| Altered mental status | Cardiac arrest |
| Apnea | |
| Neurologic symptoms typically precede cardiovascular symptoms in lidocaine toxicity | Cardiovascular symptoms typically present first in bupivacaine toxicity |
Initial symptoms may occur immediately or up to 1 hr after the local anesthetic injection.
If mild symptoms occur, monitor for 6 hr.
If severe symptoms occur, monitor for at least 12 hr after resolution.
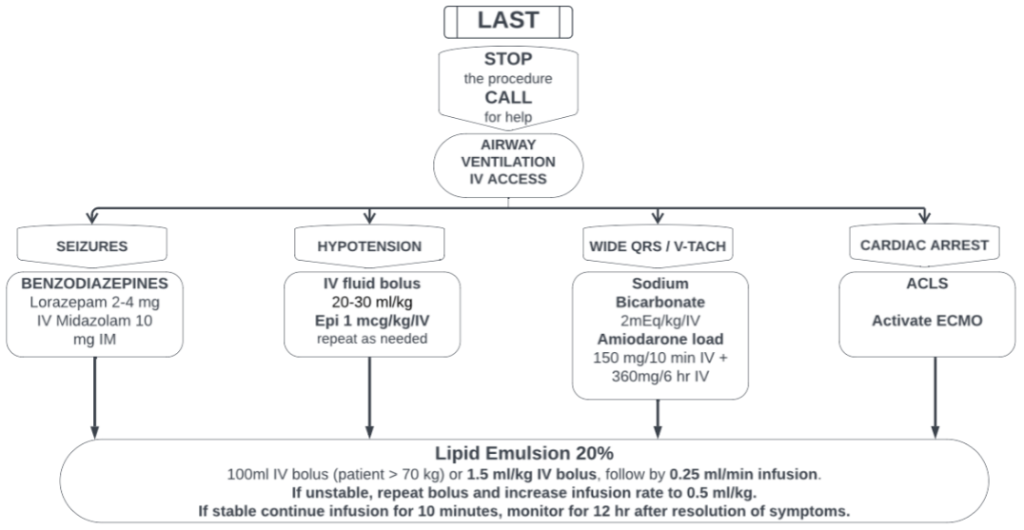
LAST treatment
Stop any procedure if minor symptoms occur. Call for help.
Maintain the Airway and Ventilation. Hypoxemia, hypercarbia and acidosis worsen the toxicity.
Establish 2 IV access. Patient should already be on a monitor.
If hypotension, give small doses of epinephrine (1 mcg/kg bolus). Avoid phenylephrine and vasopressin.
If seizures, treat with usual benzodiazepines. Lorazepam 2-4 mg/IV or Midazolam 10 mg/IM.
If wide QRS or ventricular arrhythmias, treat with sodium bicarbonate first (2 mEq/kg/bolus), repeated doses might be needed until QRS narrows. If ventricular arrhythmia persists, consider amiodarone.
With any severe symptoms, start Lipid emulsion 20%. Start with a 1.5 ml/kg of ideal weight bolus (~100 ml for a 70 kg patient), continue with a 0.25 ml/kg/min infusion for at least 10 minutes after symptoms are resolved. If the patient remains unstable, repeat the bolus and increase the infusion to 0.50 ml/kg/min. Max dose of Lipid emulsion 20% is 12 ml/kg/total, in general 1 L bag of the solution is enough to treat most of the patients.
If cardiac arrest, start ACLS. Start with lower doses of epinephrine (1 mcg/kg). Start intralipid emulsion 20% bolus 1.5 mg/kg and infusion, repeat bolus until ROSC (max total dose of Intralipid solution 12 ml/kg). Activate ECMO team early, cardiac arrest due to LAST might be prolonged (especially with bupivacaine) and there’s several case reports with good outcomes after ECMO.