Sickle cell disease affects ~ 100,000 people in the US. Though pain is the most common ED presentation for patients with SCD, we should always consider life-threatening emergencies in this devastating and complicated disease.
Acute Chest Syndrome
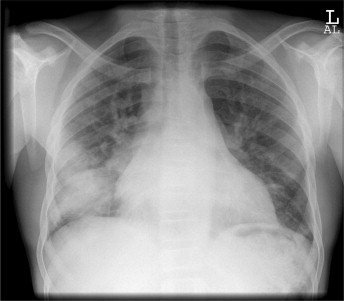
ACS is the leading cause of morbidity and mortality in patients with SCD. It’s caused by sickling in the pulmonary vasculature, leading to a cycle of hypoxia, vaso-occlusion, and consequently more hypoxia. It can be rapidly progressive and lead to ARDS and eventually death. It is easy to miss, often confused with acute pain crisis. It will often present with fever, cough, chest pain, and dyspnea. You might see pulmonary infiltrates on CXR.
In general, to differentiate from a pain crisis, ask about any associated respiratory symptoms. And any degree of hypoxia should raise suspicion for ACS.
Admit for pain control and SpO2 monitoring (> 95%). Start antibiotics (cephalosporin + macrolide).
Stroke
Both ischemic and hemorrhagic strokes may be seen with SCD. Have a high level of suspicion for patients presenting with neuro signs and symptoms. Those with low Hb, high WBC, HTN, history of silent infarcts, and history of ACS are at higher risks for stroke. CT scans may miss early signs of infarction. These are the patients you will discuss obtaining MRI + MRA with neurology.
Evaluate patients for tPA vs intra-arterial thrombolysis. Also consider that management may involve exchange transfusion and IVF instead (usually pediatric patients).
Infection
I have a very low threshold to upgrade to resus a febrile patient with SCD, regardless of age or other comorbidities. Why?
94% of patients with SCD are functionally asplenic by 5 years of age. S. pneumoniae, H. influenzae type b, non-typhi Salmonella species, Mycoplasma, C. pneumoniae and Yersinia enterocolitica are common pathogens in sickle cell patients. Etiologies to consider for febrile patients include bacteremia, osteomyelitis, or infection causing ACS.
Aplastic crisis
What about the patient that has resus-level vitals, looks pale, but does not have osteo or ACS? Is there something else we should consider?
Glad you asked. Aplastic crisis often presents with hemodynamic compromise, SOB, fatigue, and pallor. It is commonly due to Parvovirus B19 (classic Rosh review question!), so the patient may report a viral prodrome. In the ED, our care will be largely supportive, depending on the degree of anemia and cardiovascular compromise. Consider starting transfusions if retic count is less than 1-2% with goal hemoglobin of about 10 g/dL. Consult our lovely heme colleagues expeditiously. These patients will likely be admitted to the ICU.
Other emergencies
SCD is sucky. The possible complications span every organ system. They include cholelithiasis, splenic sequestration, priapism, hyphema.
**A point has to be made on how important it is to manage these patients’ care with empathy and respect. Treat their pain. And address their pain quickly and effectively. Check their charts for pain management plans, especially if they follow with Sinai’s SCD team. Reassess them frequently and involve them in your plans for dispo. **
Resources:
http://www.emdocs.net/the-sickle-cell-patient-ed-management-of-acute-complications/
