A 65 yo M is bibems tachycardic and hypotensive with one week of worsening cough and sob. Large LLL infiltrate is present on XRay. You begin treating your patient for severe sepsis and begin to wonder what has been happening in the world of sepsis recently.
October 1st, 2015:
CMS published a new sepsis bundle that we are now following at both hospitals. The bundle recreated the definitions for severe sepsis and septic shock and outlined treatment goals and timelines to achieve the same. This is listed below. They are being monitored and hospital compliance may be linked to funding in the future. These new definitions are controversial, many claiming there is no supporting evidence for portions of the bundle. Furthermore, treatment guidelines removed physician discretion which is concerning, as CHF and ESRD patients should not be receiving 30 ml/kg boluses.
Severe Sepsis:
- Suspected source of infection
- > 2 SIRS criteria
- Evidence of Organ dysfunction (regardless of pt’s baseline)
- SBP < 90 or MAP < 70 or SBP decrease of > 40 from baseline
- Cr > 2 or UOP < 0.5 ml/kg/hr for 2 hours
- Bili > 2
- Platelet count < 100
- INR > 1.5 or PTT > 60
- Lactate > 2
Septic Shock:
- Tissue hypoperfusion (defined below) persisting in the hour after IVF administration
- SBP < 90
- MAP < 65
- Decrease in SBP by > 40
- Lactate > 4
Treatment Guidelines:
- Initial 3 hours
- Resuscitate to below parameters by giving 30 ml/kg bolus (regardless of pt co-morbidities)
- CVP 8-12
- MAP > 65
- UOP > 0.5 ml/kg/hr
- ScvO2 70% or SvO2 65%
- If elevated lactate, attempt to normalize
- Draw cultures
- Administer Antibiotics (w/in 1st hour)
- Resuscitate to below parameters by giving 30 ml/kg bolus (regardless of pt co-morbidities)
- Initial 6 hours
- Apply vasopressors (for hypotension not responsive to IVF resucitation) to maintain MAP > 65
- If septic shock -> measure CVP and ScvO2
- Remeasure lactate if initial elevated
February 2016:
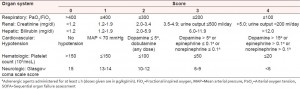
The Society of Critical Care Medicine (SCCM) published a JAMA article reformatting the definitions of sepsis. The authors attempted to update the definitions based off new understanding of the biological and clinical pathophysiology associated with sepsis. The main changes included in this paper are the removal of the term “severe sepsis”. The other major change is the use of SOFA (Sequential Organ Failure Assessment) and qSOFA (mortality predictors) as tools to replace SIRS. These guidelines are NOT endorsed by any Emergency Medicine Society and are also creating a lot of controversy. There is no discussion of sepsis treatment in this update.
Sepsis = Life-threatening organ dysfunction caused by a dysregulated host response to infection.
Septic Shock = A subset of sepsis in which underlying circulatory and cellular metabolism abnormalities are profound enough to increase mortality.
- Sepsis plus the following despite adequate fluid resuscitation:
- vasopressor required to maintain MAP > 65 AND
- Serum lactate > 2
Diagnostic tools to screen sepsis:
A patient has sepsis if an infection is suspected and rules in by one of the following criteria
> 2 of qSOFA:
- Respiratory rate > 22/min
- Altered mentation (GCS < 15)
- Systolic blood pressure < 100 mm Hg
Score of > 2 of SOFA:
Other resources on this topic:
Jeremy Faust discussing on Foamcast