You’re working in RESUS, and you get a notification for hypotension.
He’s a 65 year old male noted to be hypotensive to 70/40 by EMS. On arrival, he’s altered and unable to provide any history, and EMS doesn’t have much more information. You don’t see any signs of trauma.
Your attending suggests performing a RUSH exam to help narrow down your differential.
The RUSH (rapid ultrasound for shock and hypotension) exam is a fairly new concept, developed in effort to rapidly evaluate the undifferentiated hypotensive patient.
Think of the RUSH exam for critically ill medical patients (hypotensive, signs of shock) as the equivalent of the FAST on your trauma patients.
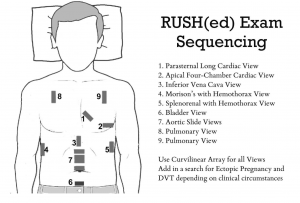
Here’s a nice graphic from EMCrit of your typical views:
And there’s a great pneumonic (also from EMCrit) to help remember this (especially since this is your end goal):
HI-MAP
HEART: look for a pericardial effusion/tamponade, RV strain (PE?), LV function (cardiogenic sources)
IVC: evaluate the volume status and guide your fluid resuscitation decisions
Morrison’s/FAST: You know what to do! This will help you assess for things like a ruptured ectopic, massive ascites, spontaneous ruptured AAA, perforated viscus.
AORTA: AAA–4 views (just below heart, suprarenal, infrarenal, just before bifurcation)
PTX: r/o tension
So next time you’re in either Resus or the Cardiac room with a hypotensive patient, grab the ultrasound and start RUSH-ing!
Shout out to Dr. Moira Carroll for inspiring this post!
SOURCES:
https://emcrit.org/rush-exam/original-rush-article/
https://emcrit.org/rush-exam/ <<< you’ll note some familiar names!