You have received a notification, EMS has a patient with “APE” or acute pulmonary edema. The patient arrives in respiratory distress and if you do nothing, she will require intubation. However, you are well practiced in the use of noninvasive ventilation and will prevent intubation today. You put the mask on the patient and start them on 10/5 and walk away right? WRONG!!!
It is obvious that non-invasive ventilation (NIV) is common practice in the Emergency Department today. As EM physicians we need to be well practiced in setting this up and understand what settings will benefit our patient. Our respiratory therapists are knowledgable but they are by no means experts. This is a brief review of basic terms and ideal settings to optimize specific patients in the department.
Bipap vs Cpap = These terms were for a different time (when machines were only capable of performing certain functions) and should no longer be used these days. NIV just makes you sound smarter and correctly describes the ventilation oxygenation strategy we are employing. Hospitals today should be utilizing machines for NIV that have both capabilities.
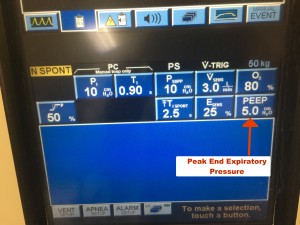
PEEP/EPAP = Peak end expiratory pressure (also sometimes referred to as expiratory positive airway pressure on some machines) is a constant pressure that is present throughout the inspiratory and expiratory cycle. It stents open the small airways and is an aid we use for oxygenating our patients. I have heard some people think that this helps patients breath out or expire. When they say this they are referring to the use of PEEP to stent open upper airway obstruction caused by soft tissue collapse when a patient sleeps at night. This is not how or why we use PEEP in the emergency department.
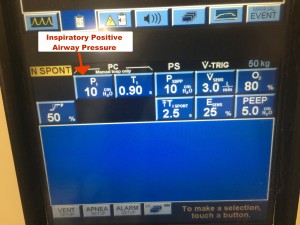
IPAP/PSV = Inspiratory Positive Airway Pressure (or Pressure Support Ventilation) is a tool we can use to aid in ventilation. As noted in the name, this pressure is only present during inspiration. It is an additional pressure that helps patients get their breath in quicker and requires less effort on the patients part to achieve similar tidal volumes (thereby decreasing their work of breathing). Please note that the vents we are using in our departments, the IPAP/PSV is additive to the PEEP (so an IPAP of 5 and PEEP of 5, really equals 10 of inspiratory support and 5 of PEEP).
FIO2 = I think this does not require further explanation but is a setting that you will determine.
Wrapping it up
Patients may require a combination of settings to help them breath.
Pneumonia/CHF patients typically have failure to oxygenate. These patients definitely need PEEP. Starting at 5 is reasonable but don’t be afraid to titrate up. These patients may benefit from some inspiratory support to aid in their work of breathing. The IPAP may increase with the PEEP but the money is PEEP in these patients.
Obstructive disease (COPD/ASTHMA) patients have failure to ventilate. These patients need IPAP to decrease their inspiratory time and allow them more time to breath out. IPAP, as discussed above, will aid in their work of breathing which is important in these patients as they will typically start to tire out as they get sicker. It is also important to remember that these patients are trapping air or auto-PEEPing. Large PEEPs in these patients can be dangerous and likely increase their chances for barotrauma. You may start these patients on an inspiratory pressure of 8 or 10 and PEEP of 0 to 2 and titrate accordingly.
Ultimately, all NIV requires patient specific adjustment. So please think about your settings and don’t just have a cardiac/resus room full of patients on 10/5.