What does the MI on the sidebar of the ultrasound machine screen stand for?
The Mechanical Index is a safety metric which lets the operator know how much energy is being transmitted into the patient during sonography. Remember that sound is created by pressure waves, Â so mechanical energy is transmitted into any object which receives sound. Sound waves can be quite powerful- remember we use them to disintegrate kidney stones and to clean jewelry. And not vice versa. So best to make sure that you are using the lowest power possible, or As Low As Reasonably Achievable, for diagnostic imaging.
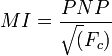
Back to the Mechanical Index. It is defined as the peak negative pressure (PNP) of the ultrasound wave (point of maximal rarefaction) measured in milliPascals divided by the square root of the center frequency (Fc)of the ultrasound wave. Not a very complicated equation, once you know the components:
What the heck is this? Think pressure change divided by time. Lots of pressure change over short periods of time can be damaging. Dr. David Toms, who writes www.fetalultrasoundsafety.net puts this into perspective very nicely. Imagine a MI of 1 in a system using a 4 MHz probe. Pretty typical parameters. That would mean a peak negative pressure of 2 MPa. According to Dr. Toms:
The corresponding positive side of the ultrasound wave would be similar in the other direction, giving an overall pressure difference within half of a 4MHz cycle of 4 MPa, equivalent to being submerged or brought up from 400 metres (1300 feet or ¼ mile) underwater in 1/8 of a microsecond. Although the 1/8 microsecond in which this 400 metre movement would occur makes the analogy impossible – it would be 10 times the speed of light – the point is to emphasize that pressure fluctuations within the ultrasound pulse are large, rapid and far from intuitively trivial.
The FDA has established a maximum MI of 1.9 for diagnostic imaging. Any machine capable of generating MI greater than 1.0 must display the MI onscreen. The FDA MI limit for obstetric sonography is 1.0.
How does this this affect care in the acute setting?
- Keep scan times to a minimum
- Avoid using pulsed wave Doppler or color flow through the fetus for determination of fetal heart rate
- Use M-Mode instead
- Use Tissue Harmonic Imaging (THI) only when necessary, not as a default setting
