Chances are you order a urine dip or urinalysis on a good number of your patients each shift. But how good are these tests at helping us diagnose a urinary tract infection?
The short answer: not fantastic.
Let’s continue, focusing on the “official UA”.
When looking at the UA results to determine if a patient has a UTI, we typically focus on the leukocyte esterase, nitrites and WBCs. Nitrites form from urinary nitrates via bacterial conversion, which most gram negative bacteria are able to do but not all gram positives have this capability. Leukocyte esterase is produced by neutrophils and may signal pyuria associated with UTI.
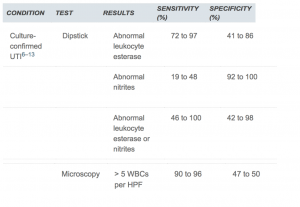
A nice review article from our friends in Family Medicine found that leukocyte esterase was much more sensitive than specific (i.e. can be positive for a number of reasons other than infection), and nitrites were much more specific than sensitive (i.e. a negative result doesn’t rule infection out). The ranges widely varied based on the study the looked at… see below!
Putting this all together, we shouldn’t be making decisions on one result alone because neither is highly sensitive or specific. Take a look at the WBC count to help you as well. They should be taken together and in conjunction with the clinical picture. When in doubt, if you are concerned about a UTI, send a culture off.
Source:
Simerville JA, et al. Urinalysis: A comprehensive review. Am Fam Physician. 2005 Mar 15;71(6):1153-1162. https://www.aafp.org/afp/2005/0315/p1153.html
Lee SP, et al. Sensitivity and specificity of urinalysis samples in critically ill patients. Anesthesiology Intensive Therapy. 2017; 49(3):204-209. https://www.ncbi.nlm.nih.gov/pubmed/28712106
SPECIAL NOTE: after writing this entire pearl, Dr. Judah Sueker informed me that he wrote a similar pearl almost exactly a year ago… So, if you want another source full of beautiful stats, click here >> https://sinaiem.org/what-the-dipstick-tells-you/