We do not encounter abdominal compartment syndrome often in the emergency department. With that said, this diagnosis enters our differential from time to time. Consider the patient with an active arterial bleed from a liver mass with large hemoperitoneum who is transferred from an outside institution for IR embolization. His abdomen is rock solid, and his lactate is 10. While you address his hemorrhagic shock, you have to at least consider the possibility of abdominal compartment syndrome. This is a case I was involved in several months ago; IR emergently drained his hemoperitoneum given the concern for abdominal compartment syndrome.
Abdominal compartment syndrome results from a sustained increase in intraabdominal pressure. The resulting decreased perfusion pressure to the viscera leads to ischemia and organ failure. While more common in post surgical patients in the ICU, this is a diagnosis the emergency physician should be familiar with.
Risk factors in ED population (this is far from a comprehensive list):
Recently post surgical
Large, tense ascites
Large hemoperitoneum (either spontaneous or traumatic)
Findings that should raise concern for abdominal compartment syndrome:
Critically ill
Tense, distended abdomen
Increased airway pressures on ventilator
Evidence of hypoperfusion to viscera (high lactate, liver dysufnction, kidney dysfunction)
Diagnosis is facilitated by measuring the intraabdominal pressure via the bladder pressure. Bladder pressure > 12 should raise concern for this diagnosis. We’ll go through the logistics of measuring a bladder pressure below.
(1) Lay the patient flat
(2) Set up a pressure transducer. Zero the transducer somewhere along the line between the iliac crest and the axilla
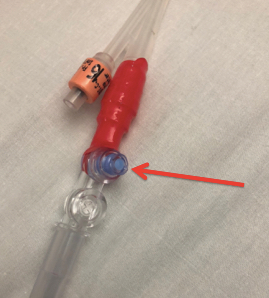
(3) Attach the pressure transducer to the blue port at the interface between the catheter and collection tubing
(4) Clamp the collection tubing distal to the port you have your transducer connected to. Make sure there is a continuous column of fluid between the port and the transducer (if there isn’t enough urine, add no more than 25 mL of saline). Allow the detrusor muscle to relax, and obtain your measurement. Pressures > 12 mmHg should raise concern for abdominal compartment syndrome in the appropriate clinical context
Pitfalls:
If the patient is in pain, the tension of their abdominal wall muscles will increase the intraabdominal pressure. Bladder pressure is ideally measured in a paralyzed patient, but we clearly aren’t going to paralyze a patient to obtain this measurement in the emergency department. If you clinically suspect abdominal compartment syndrome, involve a surgeon early in the patients course.
References:
Hunter, J. D., and Z. Damani. “Intra‐abdominal hypertension and the abdominal compartment syndrome.” Anaesthesia 59.9 (2004): 899-907.
Thanks for reading the pearls this month. See you in the ED.