It’s not just about the squeeze. You gotta think about the filling. Yes, today we’re talking about diastology (I didn’t make that word up) AKA diastolic heart failure AKA heart failure with preserved ejection fraction AKA that other heart failure.
Your patient with a history of CAD and HTN rolls in acutely short of breath. You hear some trace crackles. The xray and BNP are not slam dunk for CHF exacerbation. A chart review shows an ECHO report from last year that shows normal EF. Could this be diastolic heart failure? Is there a way to evaluate this in the ED? These are rhetorical questions, but the answer is yes. Bring your bedside ultrasound along for the ride.
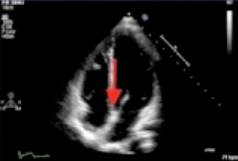
Diastology is the measure of how good the left ventricle functions in diastole. This means how good the myocardium is at relaxing and complying (blood filling up the heart). The simplest assessment involves looking at the 4 chamber view. You could look at the size of the LA and the degree of descent of the base (the red arrow below) to get a basic sense if there is any diastolic dysfunction. A large LA (>20cm^2) or poor descent of base suggests poor diastolic function.
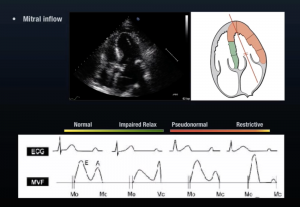
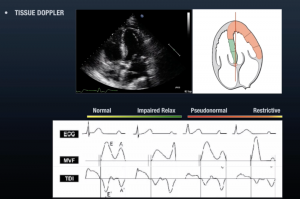
But there are more advanced methods for evaluating this on your bedside ECHO as well. These involve assessment of the mitral inflow velocity, the tissue doppler velocity at the septal annulus, and the E/E’ ratio. These terms each deserve more explanation than can be fully provided here, but know that they exist and can be measured easily on your bedside sono. Further instructions on how can be found in the links at the end. Diastolic failure is a spectrum of disease and can be broken down into a progression from normal to impaired relaxation to pseudo-normal to restrictive disease. The diagrams below show the characteristic findings as diastolic dysfunction progresses along its course.
The Ultrasound Podcast resources listed below are a much more comprehensive introduction to learning how to assess diastolic heart failure. You’ll find details and videos on how to get the views and info you need on your bedside ECHO.
Now, why do I care about this in the ED? Whether it’s systolic or diastolic failure, they are going to get treated and even potentially admitted. True. It’s not at all standard of care to diagnose diastolic heart failure in the ED on bedside ECHO right now. However, just like looking at the IVC on your bedside sono helps you get a sense of preload on the right side and guides your fluid resuscitation decisions, knowing how to look at the left side of the heart as well can help you make some point of care decisions in the management of your acutely dyspneic patient. This provides added finesse in managing your critically ill patients. Style points still count.
Sources
http://www.ultrasoundpodcast.com/tag/diastology/
http://www.foamem.com/2015/04/21/ultrasound-leadership-academy-diastology/
http://lifeinthefastlane.com/ccc/diastolic-dysfunction/