LVAD management is an appropriate topic for a fellowship; not necessarily a TR pearl. But, resuscitating the sick LVAD patient is firmly within our scope of practice, and requires some basic knowledge of LVAD physiology.
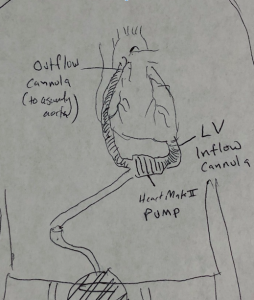
Enter rough sketch of a patient with an LVAD. Excuse my lack of artistic prowess:
There are a number of variations between LVAD models. The basic idea is, however, conserved. Each LVAD has an inflow cannula in the LV apex, a pump, and an outflow cannula implanted into the ascending aorta. The HeartMateII is probably the most common LVAD we see, and has a “driveline” that goes out to a wearable controller/battery pack.
Some patients with an LVAD have pulsatile blood flow, and some do not. This depends on a few patient-specific variables. For instance, many patients with significant aortic regurgitation have their aortic valves sewn closed to prevent a reentrant loop of bloodflow through the LVAD (blood goes into the aorta, and is sucked back into the inflow cannula). Patient with closed aortic valves do not have pulsatile flow. Patients with very poor native LV function may also not have pulsatile blood flow (or, at least, very narrow pulse pressures).
The device will give you a set of numbers once on the monitor provided by the VAD team: power, flow, and pulsatility (“PI”). Pump speed is controlled by the operator; the other numbers are dependent variables. We’ll address these in a future pearl.
Quick case:
70M s/p HeartMate II implantation one month ago presents with 3 days of weakness. MAP recorded at triage is 50.
What does this patient need:
- A blood pressure recording. There should be no delay in obtaining a MAP on an LVAD patient. But, because many patients do not have pulsatile blood flow, you can not get a reliable blood pressure reading from a non invasive blood pressure cuff. Instead, you need to use a manual blood pressure cuff with a doppler device over the brachial (or radial) artery. You simply release the pressure until you have flow, and obtain the patient’s MAP.

- Invasive blood pressure monitoring. Resuscitating an unstable patient with an LVAD requires an arterial line to obtain frequent, reliable MAP’s; have a low threshold to place one early.
- Rule out hemorrhagic shock. Patients with LVAD’s are uniformly anticoagulated, and are prone to GI bleeding (and spontaneous retroperitoneal bleeding). Rectal exam should be performed early. Point of care hematocrit may be useful.
- Evaluate for tamponade and acute RV dysfunction. These patients are at risk for tamponade. Place an echo probe on the chest early. RV dysfunction is common in patients with LVAD; the septum is pulled into the LV by the intake cannula, and becomes uninvolved in the RV’s contraction.
- Call the LVAD team. This should go without saying, and should happen in parallel with the above.
Reference:
Pratt, Alexandra K., Nimesh S. Shah, and Steven W. Boyce. “Left ventricular assist device management in the ICU.” Critical care medicine 42.1 (2014): 158-168.