When you examine the ECG of a patient who syncopized, what are you looking for? You’re probably checking for a prolonged QT interval, signs of left ventricular hypertrophy consistent with hypertrophic obstructive cardiomyopathy, a delta wave consistent with Wolff-Parkinson-White syndrome, and T-waves suggestive of Brugada syndrome. But is arrhythmogenic right ventricular cardiomyopathy (ARVC) on your differential?
Epidemiology
The prevalence of ARVC in the general population is 1 in 5000, but in some European populations, it reaches 1 in 2000. It is inherited in an autosomal dominant manner, but penetrance and expression are variable, so patients may lack an obvious family history. It is the second-most common cause of sudden cardiac death (SCD) in young people (after HOCM), and depending on prevalence in the studied population, may be responsible for up to 20% of SCD in patients under 35 years old.
Pathophysiology
The pathophysiology of ARVC on the cellular level remains unclear, but may be caused by disruption of intercellular junctions in the myocardium. Myocyte separation may cause cell death, which increases afterload and wall stress. Structurally, myocardium is replaced by fibrofatty tissue. The fibrofatty tissue slows intraventricular conduction, predisposing patients to life-threatening ventricular arrhythmias.
Signs and symptoms
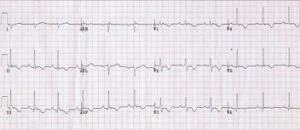
ARVC is clinically silent in childhood, and does not become symptomatic until a patient is in their 20s-40s. Unfortunately, SCD may be the first clinical manifestation. However, palpitations or syncope after physical exertion are more common presentations. These patients have ECG changes, including T-wave inversions in leads V1 through V4 and an epsilon wave – a small, positive deflection at the end of the QRS complex. While the epsilon wave is the most specific ECG finding for ARVC, it is only seen in 30% of patients.
Diagnosis
If a patient has a concerning clinical history and ECG, use imaging to confirm the diagnosis. While many patients may receive echocardiography first, cardiac MRI is more sensitive and the modality of choice.
Treatment
All patients with ARVC should avoid physical exertion, which may precipitate arrhythmias. Any patient who has been clinically symptomatic should start beta-blocker therapy. Patients who have experienced arrhythmias may consider adding amiodarone or sotalol. Patients who have had an episode of ventricular fibrillation or ventricular tachycardia should get an ICD.
References
- Corrado D, Link MS, Calkins H. Arrhythmogenic right ventricular cardiomyopathy. N Engl J Med. 2017;376(1):61-72.
- Burns E. Arrhythmogenic right ventricular cardiomyopathy. http://lifeinthefastlane.com/ecg-library/basics/arrhythmogenic-right-ventricular-cardiomyopathy/.