Given the evolving definition of sepsis and the continual push to report sepsis measures to State Health Departments and CMS, I thought the time is ripe to revisit a popular topic: the significance of elevated lactate in the ED. After all, not all elevated lactate is sepsis, and we may be able to spare some diagnostic errors in the ED by examining this popular lab value more closely.
[spacer height=”20px”]
What Causes High Lactate?
Most healthy tissues use O2-dependent aerobic metabolism for energy. Under stressful conditions when aerobic metabolism is not possible (i.e., when O2 is low), tissues switch to anaerobic metabolism, which creates lactate as a byproduct. Lactate is therefore an indicator of cellular stress.
Lactate is classically associated with hypoxia or hypoxemia (poor O2 delivery to tissues), but is actually produced under a variety of stress conditions. It is therefore more useful to think of lactate as a general indicator of impaired cellular metabolism rather than solely as a byproduct of poor perfusion.
Other markers of cellular stress, such as the anion gap or pH, are not as good as lactate. They cannot act as substitutes for lactate testing.
Healthy tissues still use anaerobic metabolism to some degree at baseline. This lactate is cleared quickly by the liver (320 mmol/L/hr), such that basal lactate levels do not rise much above 1 mmol/L. The liver does this because too much lactate can result in acidosis, which compounds cellular stress.
[spacer height=”20px”]
Why Do I Care?
Prognostication: Lactate predicts badness and whether your treatment for badness is working.
Diagnosis: It is also sensitive for occult severe sepsis (can screen for patients with high mortality risk despite being normotensive with good mental status), but not specific (lots of conditions cause elevated lactate), or 100% reliable (some patients with severe sepsis can still have a normal lactate despite being hypotensive or altered).
[spacer height=”20px”]
How Should I Order a Lactate Sample?
Don’t leave the tourniquet on for too long (which can falsely elevate the result) and trust your venous sample (it’s just as accurate as arterial). Ideally, the sample should be put it on ice if you anticipate >15 min delay to processing.
[spacer height=”20px”]
How Do I Approach the Patient with High Lactate?
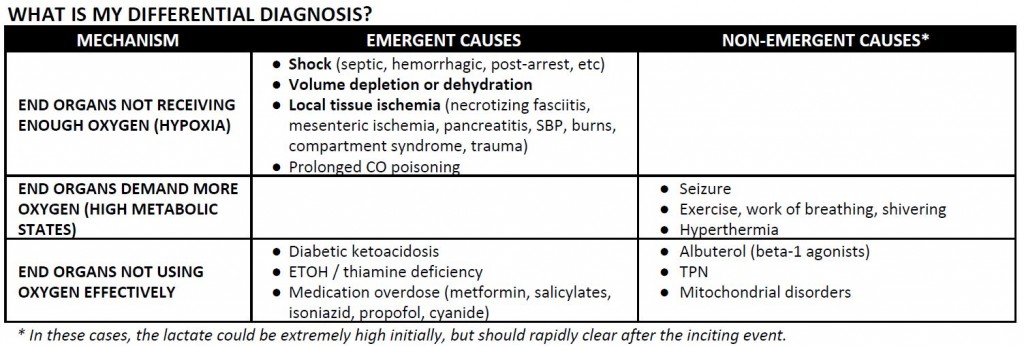
Broadly, you should split your differential into hypoxic/ischemic causes (there’s not enough oxygen to enter the aerobic pathway) versus other metabolic causes (there’s enough oxygen, but the aerobic pathway itself is impaired, inhibited, or overwhelmed). If there isn’t a clear suspected source of infection, and/or the patient has renal failure, hepatic dysfunction, diabetes, or other co-morbidities, don’t anchor on sepsis. Broaden your differential:
[spacer height=”20px”]
Similarly, in patients without a clear source of infection who have high initial lactate, consider reversible conditions upfront, including external and environmental factors such as drugs or hyperthermia that can be removed or quickly addressed. Also consider high metabolic states including heavy exercise or seizure.
[spacer height=”20px”]
What is the Significance of the Initial Lactate?
In Septic Patient: Higher mortality if initial lactate is > 4 (meets severe sepsis criteria).
In Cardiac Arrest Patient: Higher mortality if initial lactate is > 10 (92% mortality rate).
In Trauma Patient: Higher mortality if initial lactate is > 4 (84% sensitivity and 86% specificity for death).
In DKA Patient: Elevated lactate does NOT predict higher mortality.
In Liver Patient: Tread carefully. The liver is the primary organ for metabolizing lactate, but elevated lactate could be due to a secondary process (sepsis, anemia, tox) that has nothing to do with the liver. It may be useful to compare the initial value to a baseline lactate, but in general the lactate level will not be as reliable.
[spacer height=”20px”]
What is the Significance of the Repeat Lactate?
For critically ill patients, trending is most important within the first 24 hours (the “silver day” following the “golden hour”).
In Septic Patient: Less risk for badness if lactate falls to < 2.5 within 24 hours.
In Post-Arrest Patient: More risk for badness if lactate clearance < 10% within 24 hours.
In PE Patient: More risk for badness if lactate > 2 for 24 hours.
In Seizure Patient: If lactate remains elevated 1-2 hours after the seizure, consider alternative etiology.
[spacer height=”20px”]
References
- Shapiro NI, Howell MD, Talmor D, et al. Serum lactate as a predictor of mortality in emergency department patients with infection. Annals of emergency medicine. 2005 May;45(5):524–528.
- Andersen LW, Mackenhauer J, Roberts JC, Berg KM, Cocchi MN, Donnino MW. Etiology and therapeutic approach to elevated lactate. Mayo Clinic proceedings. 2013;88(10):1127-1140. doi:10.1016/j.mayocp.2013.06.
012. - Adams BD, BonzaniTA, Hunter CJ. The anion gap does not accurately screen for lactic acidosis in emergency department patients. Emergency medicine journal : EMJ. 2006 Mar;23(3):179–182.
- Blow O, Magliore L, Claridge JA, Butler K, Young JS. The golden hour and the silver day: detection and correction of occult hypoperfusion within 24 hours improves outcome from major trauma. The Journal of trauma. 1999 Nov;47(5):964–969.
- Kraut, Jeffrey A, and Nicolaos E Madias. 2014. Lactic acidosis. The New England journal of medicine, no. 24 ( 11). doi:10.1056/NEJMra1309483.