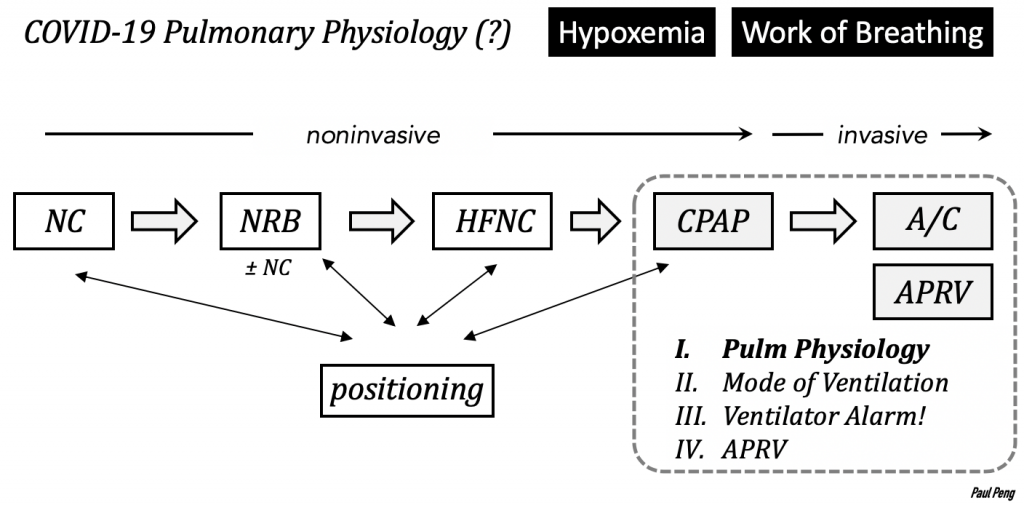
The spectrum of COVID-19 pulmonary disease is broad, perplexing, and not completely understood as of this writing. But it offers an opportunity to review fundamentals of pulmonary physiology and how it might relate to why/how our interventions (e.g. CPAP, APRV) may work.
The following is a first draft (N.B. not peer-reviewed) of my attempt at explaining some concepts of physiology, clarifying what A/C-VC actually means, and approaching vent alarms.
(Inspired by recent bedside vent management with Akash, Andres, and Chandni.) Comments/critiques appreciated.
All of this discussion hinges on understanding the origins of air FLOW.
A pressure differential or gradient is the key requirement.
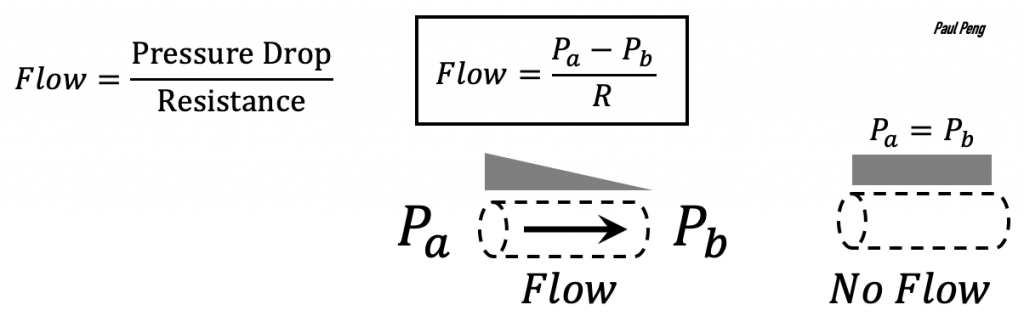
During spontaneous ventilation, the diaphragm muscles contract and the intrathoracic volume is expanded.
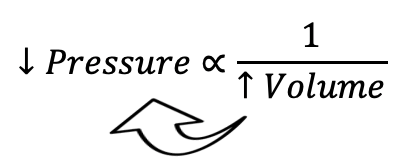
A pressure differential ∆P is generated by the decrease in intrathoracic pressure and, by extension, pleural pressure, Pout.
Flow of air into alveoli leads to an increase in volume, which depends on the compliance of the lung and chest wall system (more on this below).
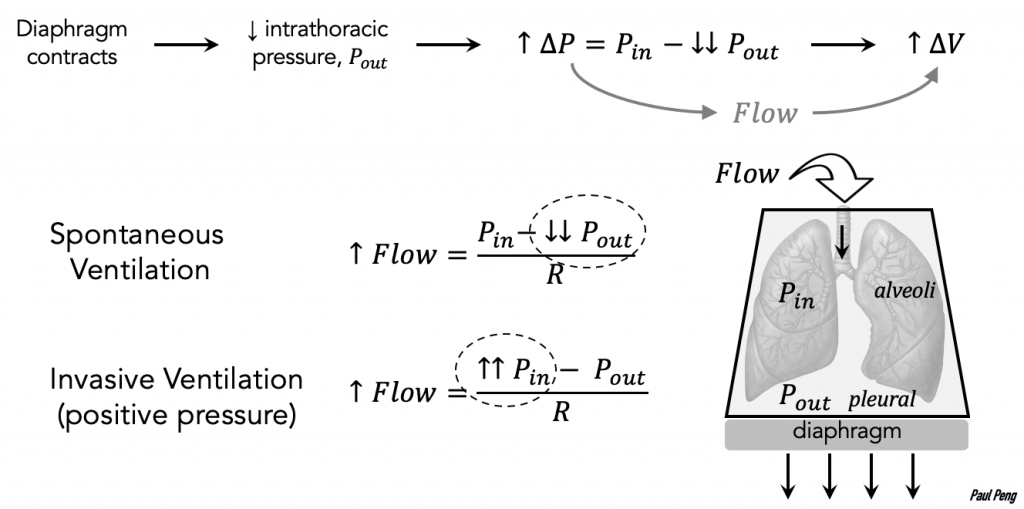
Contrast this with volume-controlled invasive ventilation, where a flow of air is delivered mechanically over time for a set volume. The alveolar pressure, Pin, generated can be rearranged from the compliance equation:
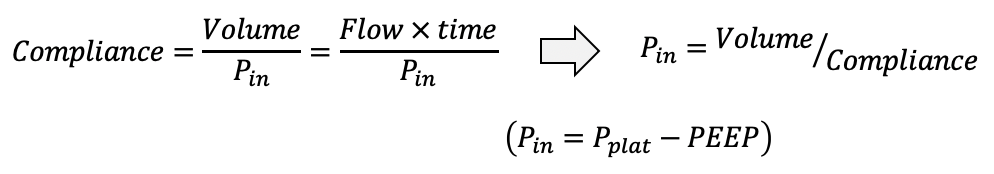
(Driving pressure is also terminology used in Pressure-Support Ventilation, corresponding to IPAP – PEEP)
Back to spontaneous ventilation…
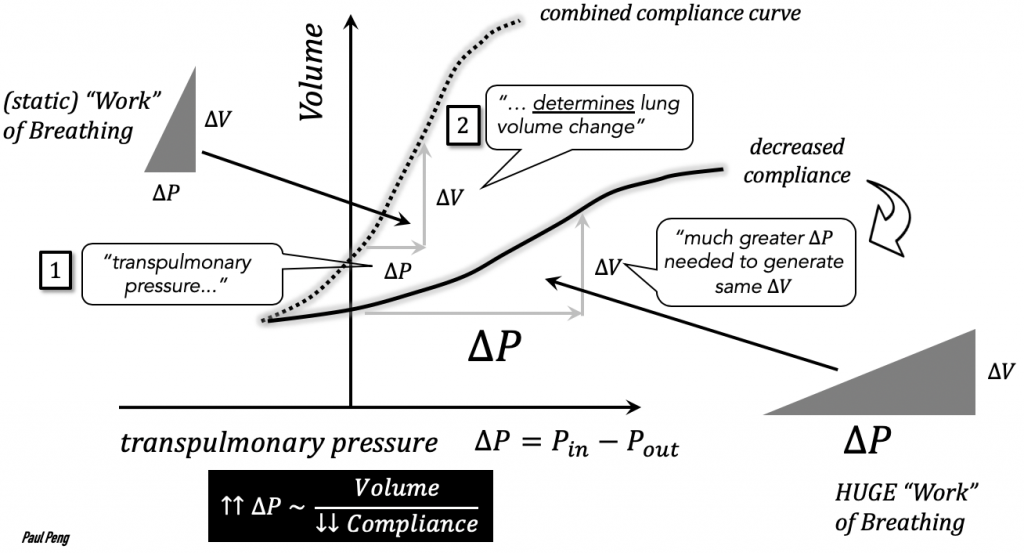
The “work” of breathing is often assessed clinically, but there is a physical basis and objective definition of work.
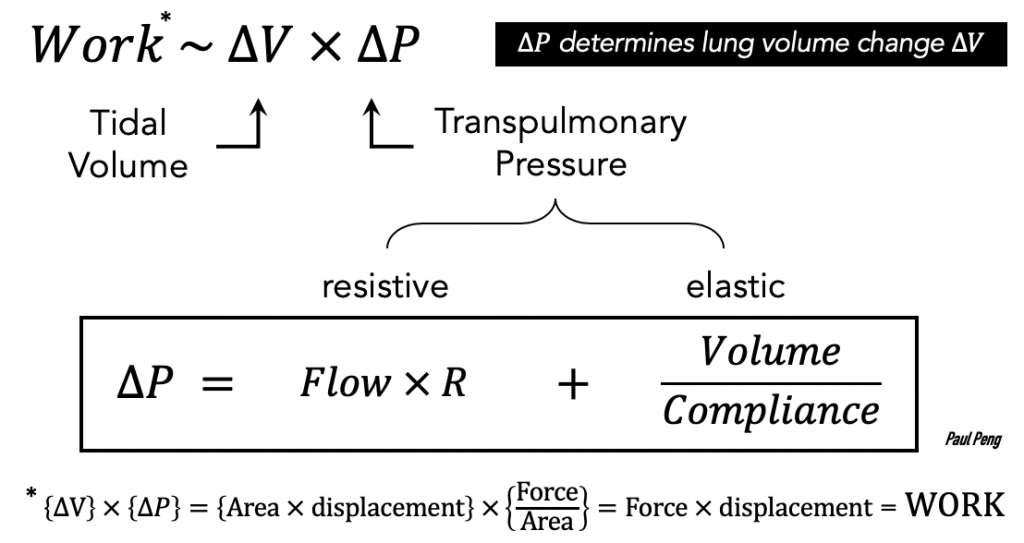
Conceptually, work of breathing is the pressure change necessary to overcome resistive and elastic work in order to generate a tidal volume ∆V.
- Key concept: Compliance refers to how easy it is to stretch the lungs.
If the lung is stiff, then compliance is low, causing the ∆P to be high. This means that a larger transpulmonary pressure necessary to generate the same tidal volume — i.e. more work!
Examine the 2 components separately:
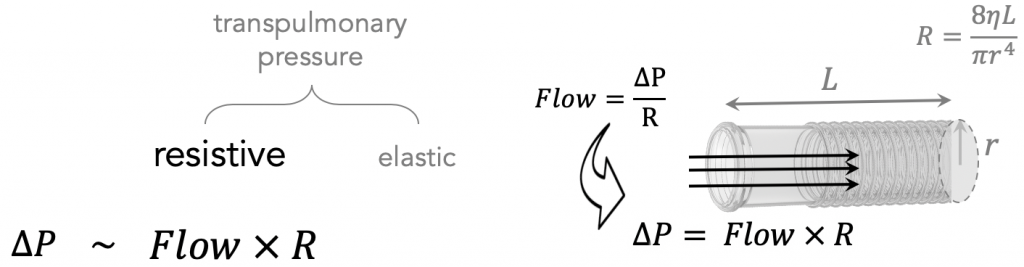
Rearranging the flow equation for pressure shows the factors that lead to increased resistance, R: small radius (e.g. bronchospasm), long tube, high viscosity.
The elastic component is slightly more complex to understand:
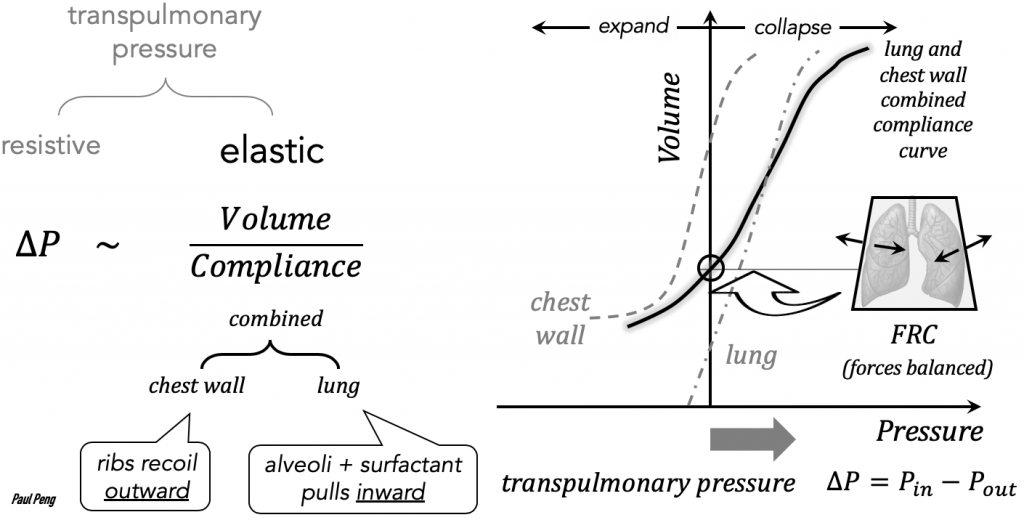
- how easily the lung stretches (i.e. compliance) depends on the balance between the chest wall (outward recoil) and the springy alveoli (inward recoil).
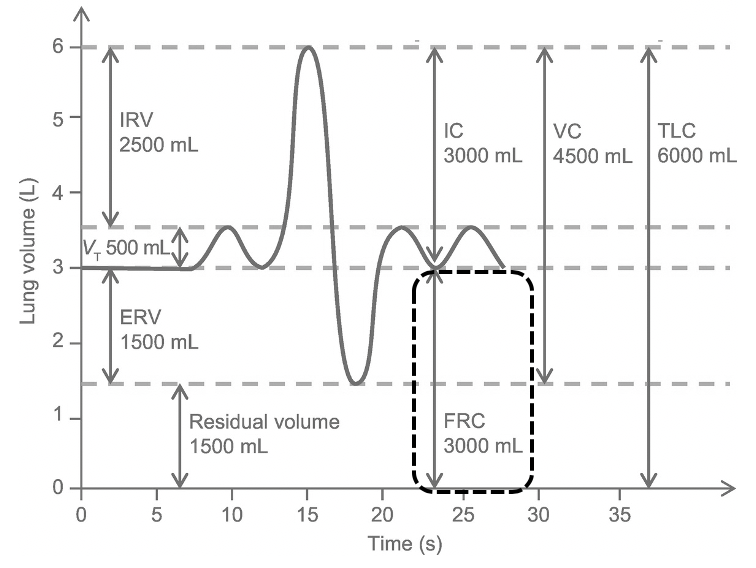
- when the recoil forces are balanced, this is the point of equilibrium known as the functional residual capacity (FRC).
- For a given transpulmonary pressure, a steeper compliance curve (i.e. easily stretched) slope generates a larger tidal volume:
Volume = Pressure × Compliance
Now it is possible to examine the “work” of breathing, comparing normal compliance with reduced compliance:
How might CPAP decrease the work of breathing (and improve hypoxemia)?
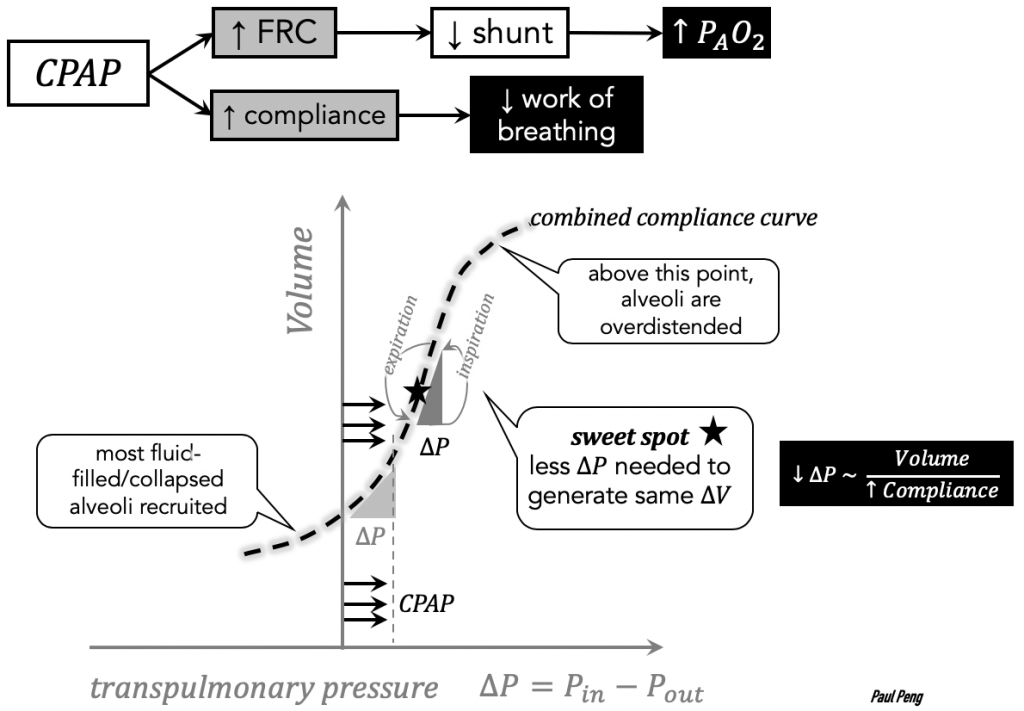
The challenge is finding the sweet spot where the slope of compliance is greatest (more bang per buck).
The compliance curve is important for understanding the theoretical benefit of airway pressure release ventilation (APRV).
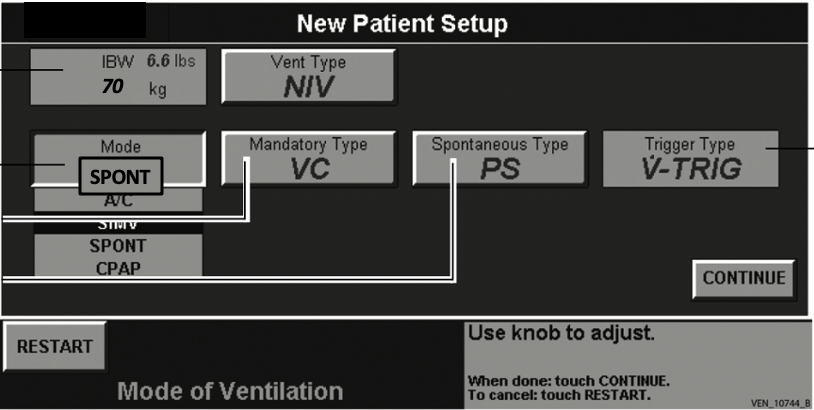
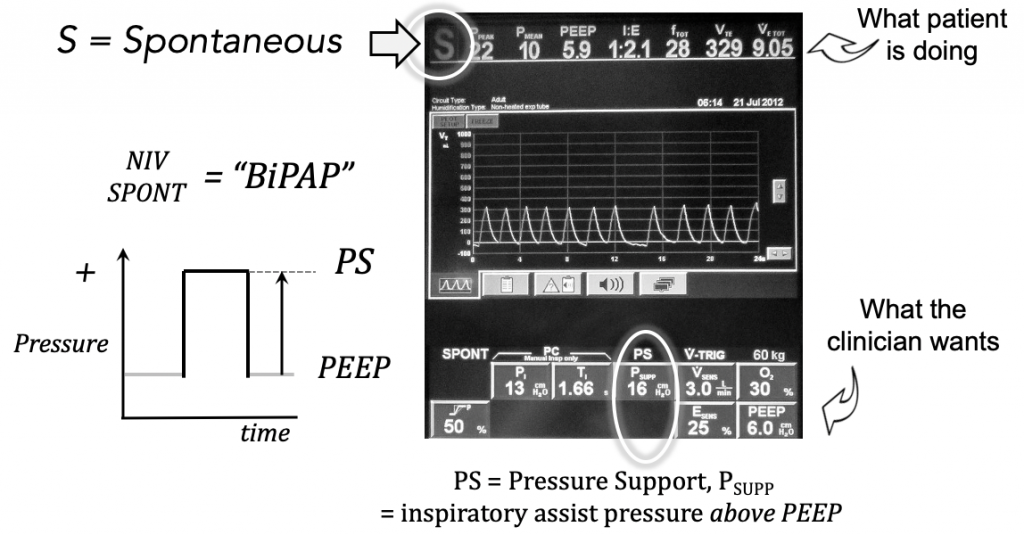
Interlude: different machines have different terminology for noninvasive pressure support ventilation (NPPV). Here is the VELA ventilator at Elmhurst and equivalent NPPV modes.
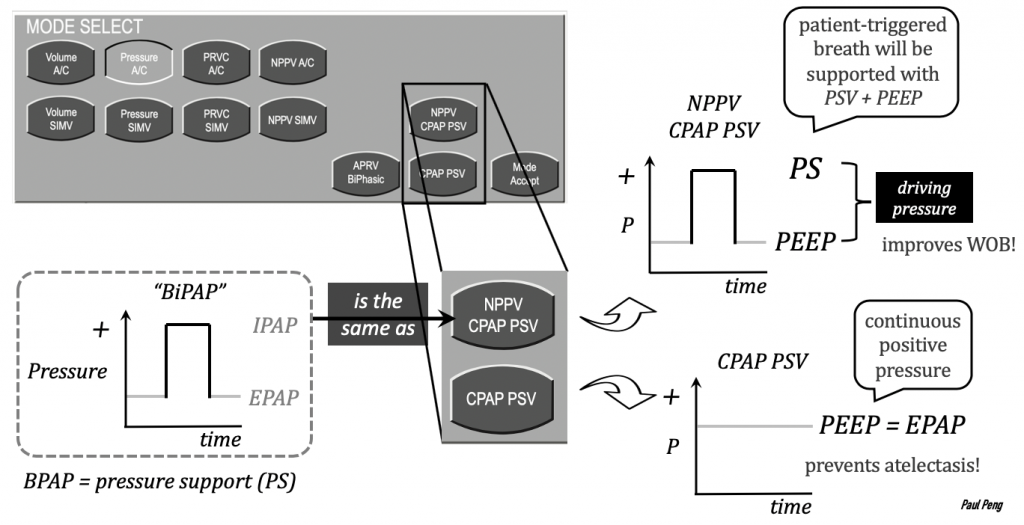
CPAP = PEEP = EPAP = CPAP PSV
I know, unnecessarily confusing.
On the Puritan-Bennett machines at Sinai:
One more thought on work of breathing. In addition to the work of generating large transpulmonary pressure ∆V, tachypnea alone could, over time, eventually cause “work of breathing”.
Often it is secondary to poor compliance leading to rapid-shallow breathing, but it could also occur during severe metabolic acidosis (trying to clear CO2).
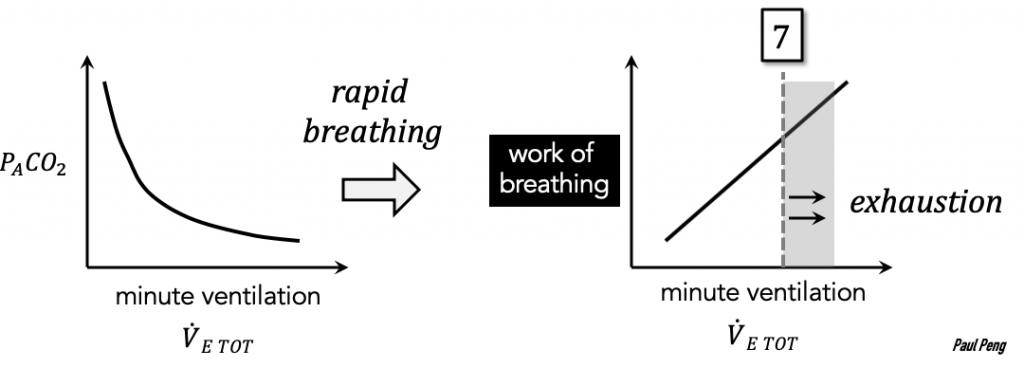
This concept has been described on PulmCrit but I have not been able to find references/experimental data demonstrating a minute ventilation >7 as being critical.
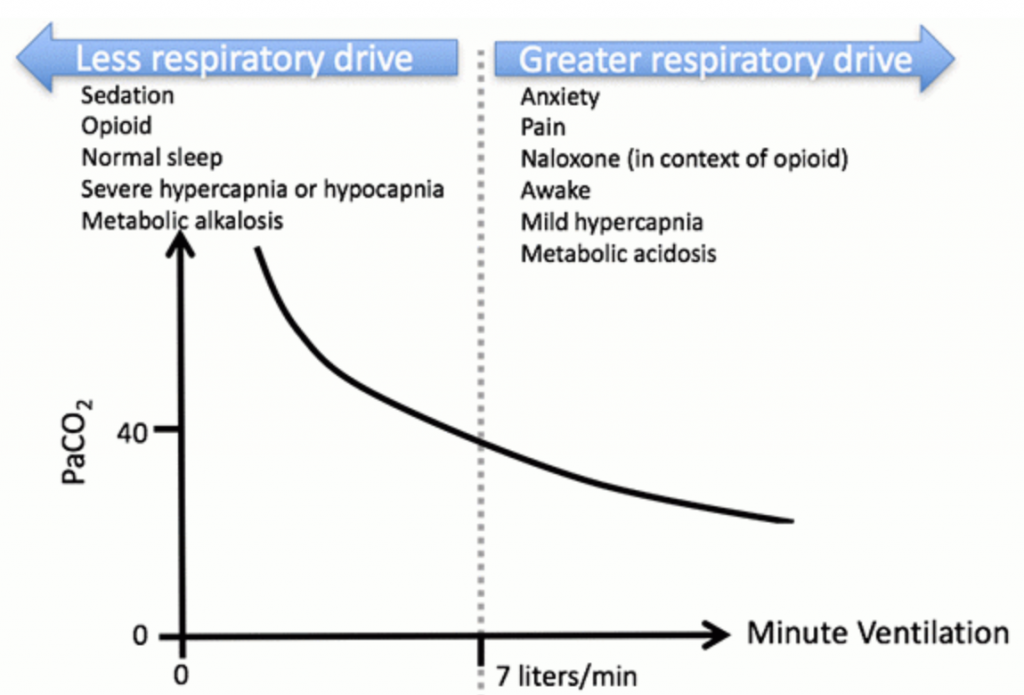
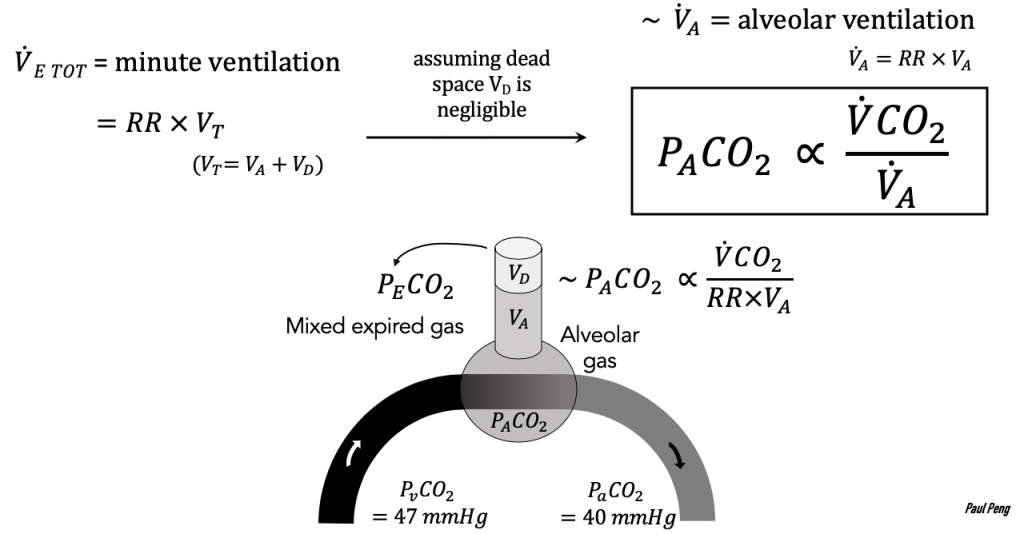
Minute ventilation represents the body’s handling of carbon dioxide, whether it be from metabolic derangements or retention.
In COVID-19 patients, it remains to be proven if tachypnea, by itself, is a reliable sign of “work of breathing”.
But according to Martin Tobin,
Tachypnea is the expected response to lung inflammation that produces stimulation of irritant, stretch, and J receptors. Respiratory rates of 25 to 35 breaths per minute should not be viewed as ipso facto justification for intubation, but rather the expected physiological response to lung inflammation. It is incorrect to regard tachypnea as a sign of increased work of breathing.
Basing Respiratory Management of Coronavirus on Physiological Principles, 2020
Next: modes of ventilation
References
Wilcox S.R., Aydin A., Marcolini E.G. Mechanical Ventilation in Emergency Medicine.
Martin J. Tobin. Principles and Practice of Mechanical Ventilation, 3e
J. M. Cairo. Pilbeam’s Mechanical Ventilation: Physiological and Clinical
Michael G. Levitzky. Pulmonary Physiology, 9e
Hooman Poor. Critical Care Lectures.
Jesse Hall. Principles of Critical Care, 4e
Scott D. Weingart. Managing Initial Mechanical Ventilation in the Emergency Department.
R Scott Harris. Pressure-Volume Curves of the Respiratory System. Respir Care 2005;50(1):78 –98
Martin J Tobin. Basing Respiratory Management of Coronavirus on Physiological Principles 2020
