This deep dive came from a question posed during a morning report by Jackson. Jackson presented the case of a patient presenting with a swollen penis at MSBI, found to have low albumin and diagnosed with nephrotic syndrome.
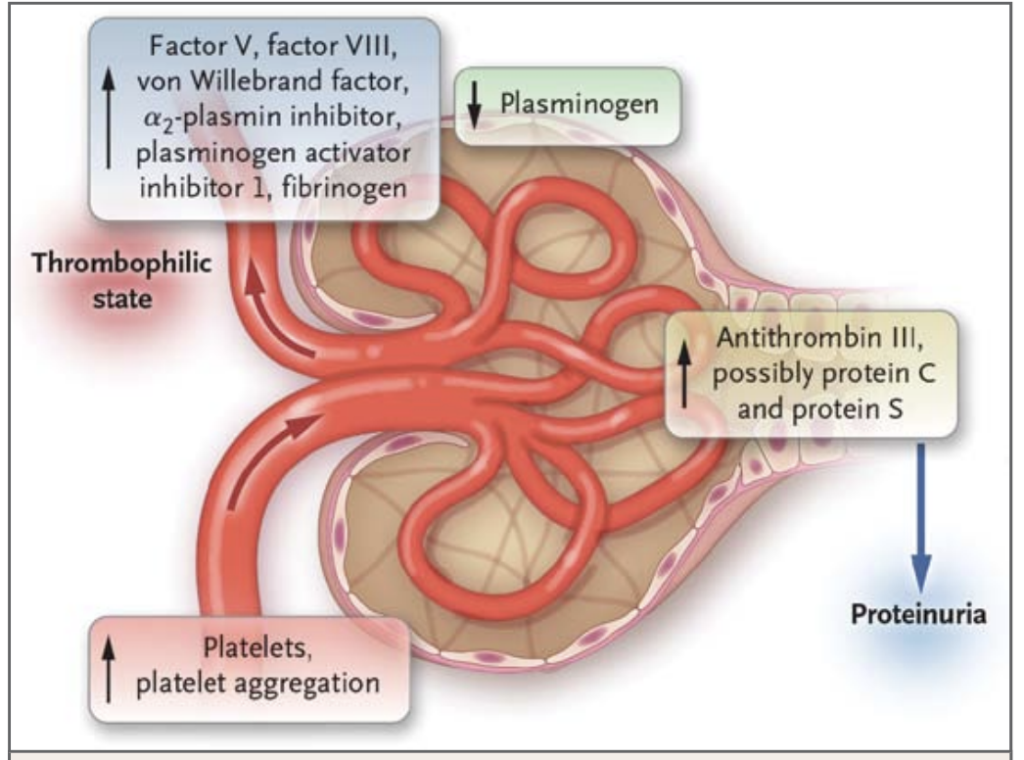
These patients are somewhat uncommon but come with interesting pathophysiology. The reason they present with edema and low albumin comes from the loss of protein in the urine. Patients excrete a variety of different proteins including anti-thrombin III, protein C, and protein S along with immunoglobulins putting them at risk for thrombosis and infection. The liver responds by synthesizing factors that cause thrombosis including factors V, VIII, VWF among others. Increased platelet activation has also been tied to certain subgroups of nephrotic syndrome. (1) This puts them at a higher risk to develop both arterial (ATE) and venous thrombosis (VTE) with up to 25% of patients developing one. (2) Some studies quote an incidence up to 51%. (3) This high rate of thrombosis can range from simple DVTs to PEs to central venous sinus thrombosis to MI. While researching this, I came across tons of reports of patients developing central venous sinus occlusions, so the risk is real.
So why does all this matter? Well, not all these patients end up getting admitted. Many might prefer to follow up with their PCP. At Sinai, some of these patients can probably go home if they have mild symptoms or after a short RETU stay if they have good nephrology follow-up. If we do send them home, it is important to identify which of these patients are at the highest risk for ATE or VTE. One paper found urine protein (8.2 g/d measured both with a spot estimate and over 24 hours) and proteinuria to albumin ratio (5.6) as cutoffs for increased risk for VTE. (4) Other papers show similar risk though exclusively with 24-hour urine collection. (5) This may present a value to help base anticoagulation decisions on discharge along with other risk factors for VTE. It’s important to note this didn’t look at an ED population so it may not be as applicable. A 24-hour urine collection is not feasible in the ED, but it may be possible in an obs unit.
There are no good prospective trials that indicate who we should consider anticoagulation, and the decision is largely up to the provider. There are two studies that seem to get cited the most. One is from Denmark which is a retrospective study of patients with biopsy-confirmed nephrotic syndrome. It showed that patients who were anticoagulated had a decreased risk of clinically significant thrombosis but had more bleeding episodes. (6) It’s important to note that the episodes of major bleeding occurred in patients receiving anticoagulation and aspirin. The other is a retrospective study from Sweden which showed that patients with severe hypoalbuminemia were at increased risk for VTE and bleeding. Importantly, this study did not show that patients who were anticoagulated had decreased risk of VTE (7).
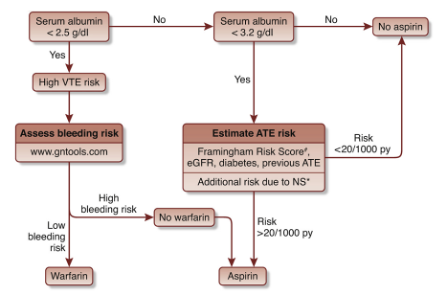
If we choose to anticoagulate, what should we choose? I don’t really have a good answer to that. The Swedish study included patients using DOACs, but mostly, we just have case reports of patients using DOACs with success (8) which I find it hard to base decisions off. I found a paper that provided a possible algorithm to decide whether to use warfarin vs aspirin (9) but this isn’t as applicable to a discharged ED patient since we are not going to be discharging a patient on warfarin. The Danish study looked at the use of Lovenox and warfarin so again, it may not be as applicable, and with the bleeding risk increased on those already on aspirin, I would be very careful.
So where does this leave us? This probably makes me more likely to admit, or at least obs, patients presenting with possible nephrotic syndrome given their presumed risk of VTE and ATE and in the absence of good data on prophylaxis. I don’t know if I feel entirely comfortable sending this type of patient home, but with very good follow-up, and a discussion of risks vs benefits, I could see myself making the decision to start them on a Lovenox or a DOAC in very, very selected cases.
References
(1) Mechanisms of hypercoagulability in nephrotic syndrome associated with membranous nephropathy as assessed by thromboelastography. Thrombosis Research. 2015.
(2) Venous Thrombosis in the Nephrotic Syndrome. NEJM. 2013.
(3) Acute ischemic stroke associated with nephrotic syndrome: Incidence and significance — Retrospective cohort study. eNeurologicalSci. 2015.
(4) High Absolute Risks and Predictors of Venous and Arterial Thromboembolic Events in Patients With Nephrotic Syndrome. Vascular Medicine. 2007.
(5) Risk factors for predicting venous thromboembolism in patients with nephrotic syndrome: focus on haemostasis-related parameters. International Journal of Nephrology. 2014.
(6) Prophylactic anticoagulation in nephrotic syndrome prevents thromboembolic complications. BMC Nephrology. 2019.
(7) Prophylactic anticoagulants to prevent venous thromboembolism in patients with nephrotic syndrome—A retrospective observational study. PLOS One. 2021.
(8) Use of Rivaroxaban in a Patient With History of Nephrotic Syndrome and Hypercoagulability. Annals of Pharmacotherapy. 2014.
(9) Should aspirin be used for primary prevention of thrombotic events in patients with membranous nephropathy? Kidney International. 2016.
