The Case:
A woman in her twenties with no significant medical history presents with one month of progressive frontal headaches radiating to her occiput. Her headaches have been intermittent, however over the past few days she has had a few episodes of vomiting and brief episodes of blurred vision. Her headache is 8/10 currently. Last emesis and blurred vision were both 12 hours prior. She was seen in urgent care for these headaches two weeks ago, and was prescribed naproxen, which has not significantly improved her symptoms. She denies fevers, chills, neck pain, focal weakness or numbness, dizziness, or trauma; and denies history drug use or a family history of cerebral aneurysm, SAH, or AVM. She immigrated from South America a few years ago.
Normal neuro exam. Steady gait. No nuchal rigidity. PERRLA, EOMI, and normal Snellen Exam.
Her urine pregnancy is negative. Her symptoms are not relieved with acetaminophen, metoclopramide, and IV fluids.
As you debate broadening your headache cocktail vs obtaining a CTH, you grab the POCUS to measure her Optic Nerve Sheath Diameter (ONSD).
Review of POCUS to measure ONSD
POCUS 101 and 5 Minute Sono have great tutorials with step-by-step instruction
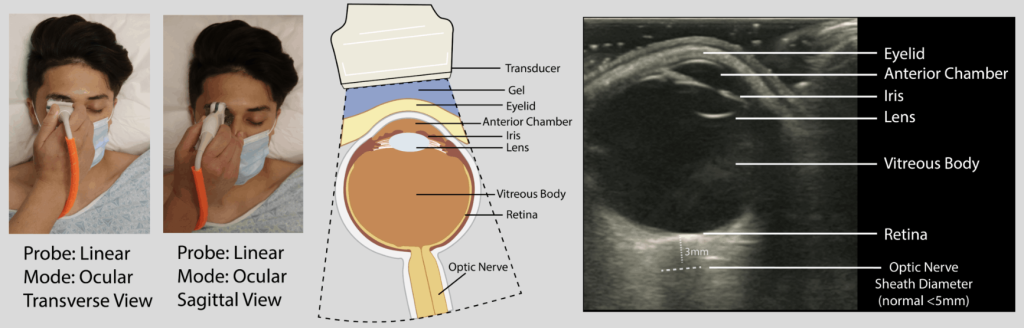
Image Credit: POCUS 101
- Place patient supine, HOB 30-45 degrees, eyes closed +/- Tegaderm (remove air)
- Apply lots of gel
- Superficial, linear transducer in transverse orientation
- Anchor hand on maxillary or nasal bone to avoid placing pressure directly on eye
- With lens in view, fan up and down until hypoechoic optic nerve is in view
- May need to rock probe slightly lateral to optimize view
- Measure the ONSD 3 mm deep to where the optic nerve sheath engages the retina
- >5 mm is considered abnormal
- think of a 3 x 5 notecard to remember these two measurements
- Repeat on contralateral side
- Additionally, look for papilledema (also called the crescent sign)
- Consider repeating these steps and obtaining an average of 3 measurements
- If two linear hypoechoic structures seen, the outer border is the optic nerve sheath
Image Credit: POCUS 101
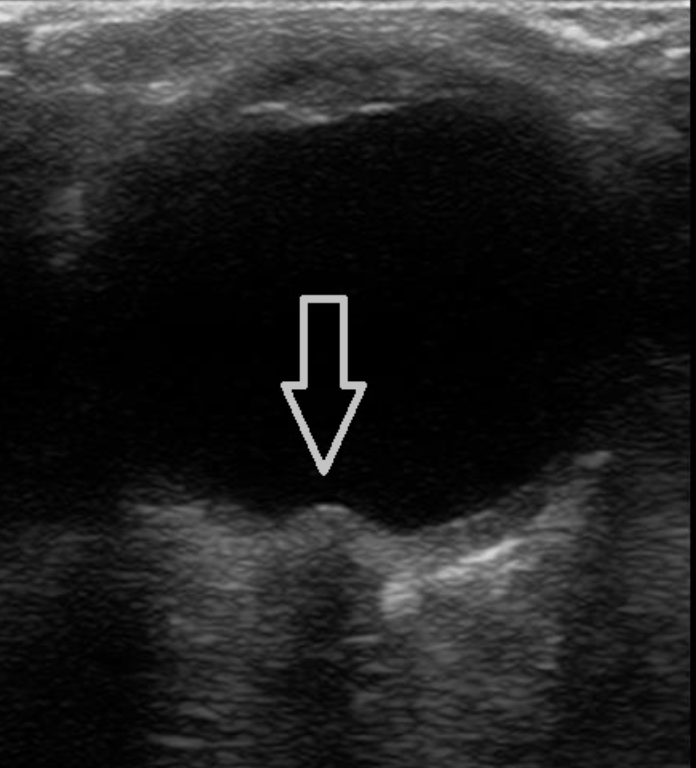
Papilledema “crescent sign” on ocular ultrasound. Image Credit: POCUS Toronto
Contraindications to Evaluation: Globe rupture
The Evidence:
A meta-analysis (Ohle et al., 2015) of 12 studies with 478 patients found a sensitivity of 96% and specificity of 92% for elevated ICP, as compared to CT.
A meta-analysis (Aletreby et al., 2021) of 16 prospective studies with 619 total patients found a sensitivity of 90% and specificity of 85% for elevated ICP, as compared to invasive ICP monitoring. ICP and ONSD had a correlation coefficient of 0.7. All studies defined elevated ICP as >20, however ONSD cutoff varied from 4.8 mm to 6.4 mm.
The largest meta-analysis to date, Koziarz et al., 2019, included all ages and any reference standard. Included 71 studies with 4551 patients with a sensitivity of 97% and specificity of 86% in the traumatic brain injury subgroup, and 92% and 86% in non-TBI patients. Very heterogeneous group of studies compared to above.
These meta-analyses all varied in terms of what their ONSD cutoff was.
Given the high degree of variability in cutoffs, another meta-analysis, (Kim et al., 2019), of 6 studies with 352 patients, established a single ONSD cutoff of 5 mm to detect elevated ICP. This cutoff had a sensitivity of 99% and specificity of 73% for elevated ICP.
As expected, as you decrease the optic nerve sheath diameter cutoff, you increase the sensitivity and decrease the specificity of elevated ICP; and vice versa.
As with any test, we should have a Bayesian mindset. Have a pretest probability in mind, and then adjust it in accordance with our subsequent tests.
There is broad agreement that ICP is generally normal if ONSD <5 mm, and that ICP is increased if > 6 mm.
As Kim et al shows, ONSD of 5 mm is quite sensitive for ICP elevation, but not very specific.
Josh Farkas in a PulmCrit blog post proposed an algorithm that incorporates both ONSD and papilledema, anticipating it to be most accurate with critically ill patients.
Here is a very comprehensive narrative review of the optic nerve POCUS (Lau et al., 2023).
And back to our patient . . .
Her ONSD was elevated bilaterally to 6.4 mm. This prompted further imaging and work up. The top of my differential was idiopathic intracranial hypertension vs possible intracranial mass vs cerebral venous sinus thrombosis.
The CTH showed scattered parenchymal and extra-axial calcifications and cysts. MRI brain showed multiple contrast enhancing regions and scattered extra-axial calcifications with surrounding edema – concerning for active neurocysticercosis. CTA H/N neg. MRV neg. LP confirmed elevated ICP (opening pressure 40). She was admitted for a few days and was further found to be strongyloides positive. She was later discharged on prednisone, levetiracetam, albendazole, and praziquantel. Seven months later her MRI showed significant improvement, and a few months later all of her medications were safely discontinued.
