The Case: A 50 year old male presents to the emergency room with complaints of shortness of breath. He appears altered, and is not able to provide more history. There is no collateral information available in his chart. Labs reveal a glucose of 300, lactic acid > 15, ph 6.9, + anion gap. Patient is intubated, and given 1L of NS. He is empirically treated for sepsis with broad spectrum antibiotics. The providers have a concern for DKA, and are going to start and insulin drip, but the post intubation VBG shows glucose in the 200s, ph is 7.2, and lactic acid is now 6. While waiting for an ICU bed in the ED, lactate uptrends to 7.8. Poison control is consulted, and confirm the diagnosis. Metformin poisoning.
French lilac was initially used to treat diabetes in medieval Europe. The active ingredient, guanidine, was used to synthesize other antidiabetic agents in the 1920s and biguanides (i.e phenformin and metformin) became available for clinical use in the 1950s. Metformin is one of the most commonly prescribed diabetic medications in the world. Metfomin alone does not lead to hypoglycemia, as metformin is an anti-hyperglycemic agent.
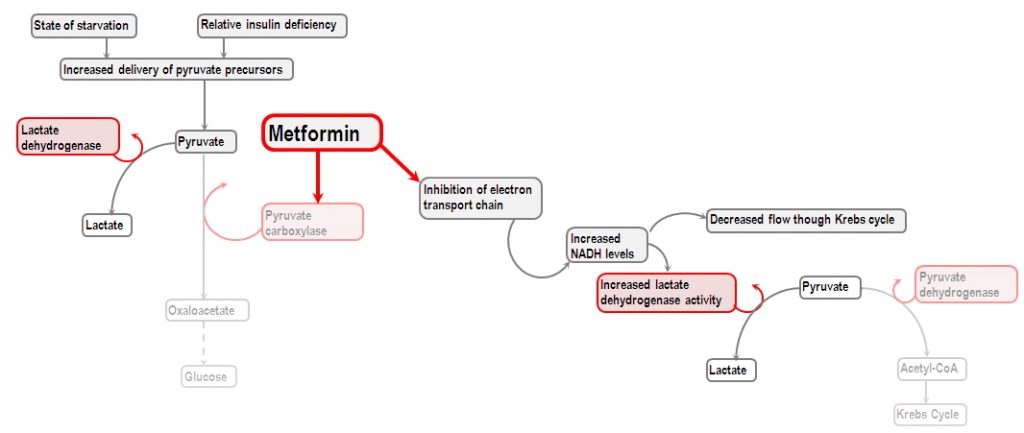
The major toxicity of metformin is lactic acidosis. Metformin promotes the conversion of glucose to lactate in the splanchnic bed of the small intestine. Metformin also inhibits mitochondrial respiratory chain complex 1, leading to decreased hepatic gluconeogenesis from lactate, pyruvate, and alanine. This results in additional lactate and substrate for lactate production.
When should you worry about metformin toxicity?
There is no clear dosage of metformin that has been associated with toxicity. The clinician should have a high index of suspicion for toxicity in children who ingest more than one or two tablets or anyone who presents with intentional overdose. Chronic toxicity can occur in patients with comorbidities such as renal insufficiency, liver disease, or heart failure.
History and Physical Exam
While history may be unreliable in this situation, determining dosage, and coingestions can be useful. Often these patients will complain of nausea, and abdominal pain. In chronic overdose and in metformin associated lactic acidosis (MALA), complains include nausea, vomiting, and diarrhea, followed by altered mental status, shortness of breath, and hypotension.
Laboratory Evaluation
Obtain all of the labs you would usually for an overdose (tylenol, salicylates, alcohol level, etc.). ECG, and a fingerstick to evaluate for hypoglycemia. Serial blood gasses are helpful to evaluate patient’s acid base status. Metformin concentration is unhelpful, as serum concentration does not correlate with severity of poisoning or patient’s outcomes. The test is also not readily available at most hospitals.
Treatment
ABC’s first! If the patient requires intubation, remember to try and closely match their minute ventilation prior to ventilation, as they may be trying to compensate for their metabolic acidosis. You can consider giving activated charcoal to your patients with known acute ingestion, as long as there are no contraindications (bowel perforation, aspiration, etc.). If the patient becomes hypoglycemic, IV dextrose 0.5 to 1g/kg is recommended. Sodium bicarbonate administration is controversial, but can be considered in severe acidosis (ph less than 7.15). Ultimately these patients will require extracorporeal removal of metformin with dialysis. There is no antidote for metformin poisoning.
Case conclusion: Patient had a Shiley catheter placed in the ED, was taken emergently for hemodialysis and admitted to the MICU.
