Today we’ll be discussing acute kidney injury (AKI). How often are you looking at the Bun/Cr thinking ‘Patient has an AKI’…and then not much more? I’ve done this. While ascertaining the underlying etiology is not always necessary in the ED, understanding AKI management, principles, and follow-up are important given the increased risk for progression to CKD and increased mortality (This has also prompted further evaluation and early recognition (using Machine Learning?)
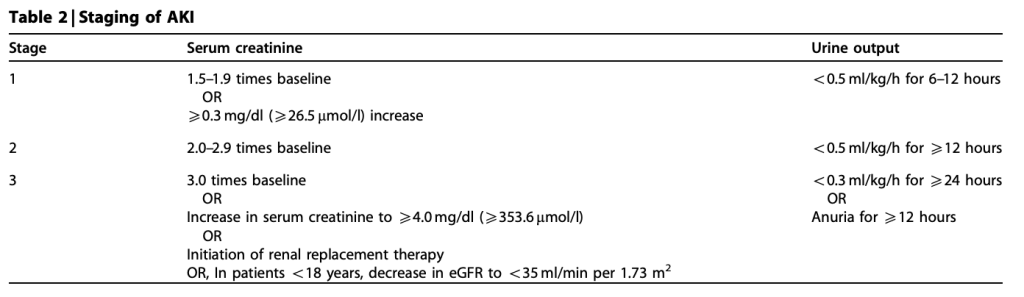
What is an AKI? Sudden, potentially reversible kidney dysfunction with dysregulated glomerular filtration leading to electrolyte imbalance and nitrogenous waste retention. (If this persists for 3 months, it’s chronic kidney disease). There are many definitions of AKI, most people use the KDIGO (Kidney Disease: Improving Global Outcomes) criteria which are:
- Increase in serum creatinine by ≥0.3 mg/dL within 48 hours; or
- Increase in serum creatinine by ≥1.5 times baseline within seven days; or
- Urine volume <0.5 mL/kg/h for six hours
Ok, now we know what it is. There are 3 types of AKIs: prerenal, intrarenal, postrenal. While many specific disease processes can lead to each, we’ll focus on categories. Prerenal (BUN/Cr > ~20) is frequently caused by hypovolemia, hypotension, shock, Renal artery vascular disease (i.e. aortic dissection or renal artery stenosis, (& many others). Intrarenal (BUN/Cr typically normal ~10-15) causes include interstitial diseases (think infection, autoimmune, or infiltrative), glomerular diseases, and nephrotoxins. Finally, postrenal (BUN/Cr variable) etiologies include intraluminal obstruction (i.e. calculi or vesicoureteral reflux), extrinsic compression (i.e. BPH or malignancy) trauma, or spinal cord injury. There are many other causes but working up Wegener’s Granulomatosis, neurogenic bladder, etc does not need to be completed in the ED.
So what should we definitely be doing? Depending on what you’re concerned for, the workup can include:
- Labs – Serum chemistry, CK, BUN/Cr ratio, FeNa, Specific gravity, Microscopic analysis, Urine electrolytes
- EKG – evaluate for changes secondary to electrolyte changes
- CXR – volume status, infection
- KUB – displaced ureteral stents, nephrolithiasis
- U/S – hydronephrosis, hydroureter, bladder distention, flow doppler of the kidney
- CT – nephrolithiasis, abdominal/pelvic masses
An EM Cases Podcast recommends a 5 step approach:
- Rule out immediate life threats: Hyperkalemia & severe acidosis (VBG & electrolytes)
- Assess for adequate perfusion: Are they in shock? H&P & POCUS
- Assess for pulmonary & peripheral edema. Here, they recommend
- AKI with adequate perfusion + pulmonary edema (with or without peripheral edema)
- Give furosemide 1 mg/kg IV (or 1.5 mg/kg IV if on furosemide already)
- Think about pulmonary renal syndromes other than CHF (such as anti-GBM disease, ANCA associated vasculitis, circulating immune complex syndromes like lupus), and look for clinical clues (inflammatory arthritis, purpura, Raynaud’s, mononeuritis multiplex, uveitis or Sicca syndrome?)
- AKI with adequate perfusion, with peripheral edema but not pulmonary edema
- Give furosemide 1 mg/kg IV (or 1.5 mg/kg IV if on furosemide already)
- If no improvement in renal function think about hypovolemia (“pre renal”) despite peripheral edema
- Low serum albumin – treat underlying cause, and consider hepatorenal syndrome which may require IV albumin
- Venous insufficiency and/or lymphedema – give crystalloid, consider compression therapy
- Drug-induced edema – give crystalloid, reassess offending drug
- Severe myxedema – give L-thyroxine and monitor
- AKI with adequate perfusion + pulmonary edema (with or without peripheral edema)
- Measure PVR, urinalysis, monitor urine output, avoid nephrotoxic agents
- Consider imaging, especially if concerned for post-renal causes
Treatment of underlying etiology, correcting electrolyte abnormality, & optimizing patient volume status/shock status. This can include volume resuscitation, relieving obstruction, avoiding nephrotoxic medications, & considering dialysis. While isolated AKIs may be discharged if otherwise appropriate, it’s important to make sure they have reliable follow-up for their AKI. This 2017 paper showed that EDs are not great at providing follow-up for isolated AKIs (caveat: small sample size). Admitting for further workup, especially in the setting of comorbid conditions is necessary to identify the underlying etiology & monitor for resolution of AKI. For more on this topic and specific recommendations for oliguria, furosemide stress test, and when to use bicarb, see here. Importantly, newer prospective studies show that FENa is not a great measure of volume responsiveness in oliguric patients.
There you go! A brief discussion of what AKI is, what types of AKIs exist and some underlying diseases, a workup schema, and some reading at the hyperlinks for a deeper dive!
Yours in learning,
Shivam
