Opioids and why
Written by Erena Weathers
Case: you have someone who broke their leg doing a ~*~sick~*~ skateboard trick. They stuck the landing, and their tib-fib snapped. They’re ready to be discharged and you feel like the good ‘ol Tylenol/Motrin won’t be enough to get them through the next couple of days. You decided let’s do an opioid. You know to be wary, but you also don’t know the best option.
1st let me drop these conversion tables. We normally give IV medications in the department, but we are not sending patients home on IV medications.
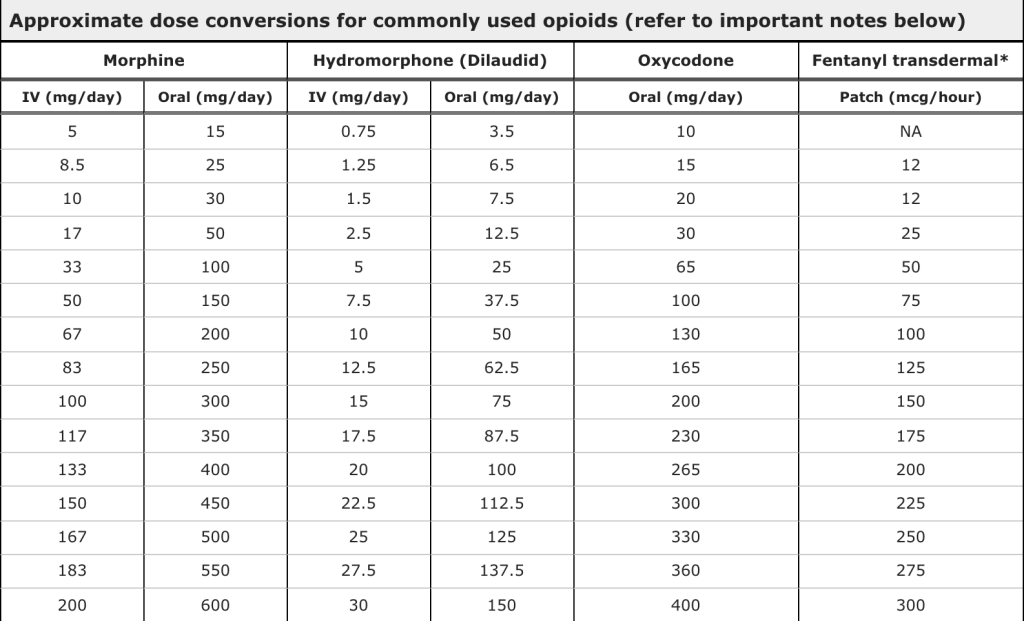
So we first have the ol’ reliable Percocet. The usual formulation is 10mg oxycodone and 325 mg acetaminophen. The oxycodone can range from 5mg to 20mg. This medication is dosed q4-6h prn. This medication obviously has a high abuse/dependence potential due to the oxycodone aspect. But what about the acetaminophen aspect? It isn’t even the therapeutic dose of acetaminophen. When we give patients Tylenol, we are usually giving 975mg or 1000mg per dose. In that scenario to reach an acetaminophen therapeutic benefit with a Percocet, you would need to give three 5/325 just to reach the acetaminophen benefit. That is the same as 8.5mg of morphine with 1gm Tylenol. When was the last time you did that in the ED? Or even worse, you’re prescribing the 10mg or even 20mg dose of Percocet, then you’ll need to be giving up to 30mg or 60mg of oxycodone PO to reach the acetaminophen therapeutic level that’s 17-30mg IV morphine equivalents.
Another downside of Percocet and any combination narcotic is the patient may supplement their medication with OTC Tylenol. This increases their risk for acetaminophen toxicity. Not good.
But Erena, this is what ortho is telling me to prescribe. Yeah well, opioids aren’t bones, so I’m not going to listen to them. Also when was the last time an orthopod pushed Narcan?
I am switching to PO immediate-release morphine for my patients that need 2-3 days of higher-level pain management and are opioid-naive. This is after reading through Strayer’s EM:Rap episode June 2018 and his paper “Something for pain: responsible opioid use in emergency medicine” in The American journal of emergency medicine. The downside is that PO morphine is not as common as percs, so you may get some pushback but every consult note says “pain management as per ED team” so go for it. The evidence is limited that IR morphine has less addictive potential than IR hydrocodone or IR oxycodone, but it is there. Strayer also combed through drug use boards, and opioid users discussed less of a high from the IR morphine than oxy/hydrocodone.
Let’s not even broach Tylenol-3 (codeine is trash), or tramadol (also trash). These drugs are so variable in their metabolism and vary from person to person that it is hard to ensure you’re achieving appropriate analgesia without horrible side effects. Also, shut down people who say tramadol is safe. It can cause dependence and withdrawal, seizures, and serotonin syndrome.
So while no opioid is safe, we can try to mitigate the damages. Discuss with patients multimodal pain relief with NSAIDs/Tylenol and then PO morphine for breakthrough pain. Also, discuss the abuse potential, and you are looking out for them by not prescribing 30 tabs for their broken leg. Also, discuss the support available if they find themselves with a dependence problem. Going back to the man of the hour (the hour it took me to write this), Strayer, he has a nice page on his site with helpful cards and instructions when giving patients opioids.
