(Previous posts: work of breathing, mode of ventilation, ventilator alarms)
NOTE: this is NOT a peer-reviewed post (pending) and is continuously under construction on the sinaiem.org website!
(Last update: 4/18/20)
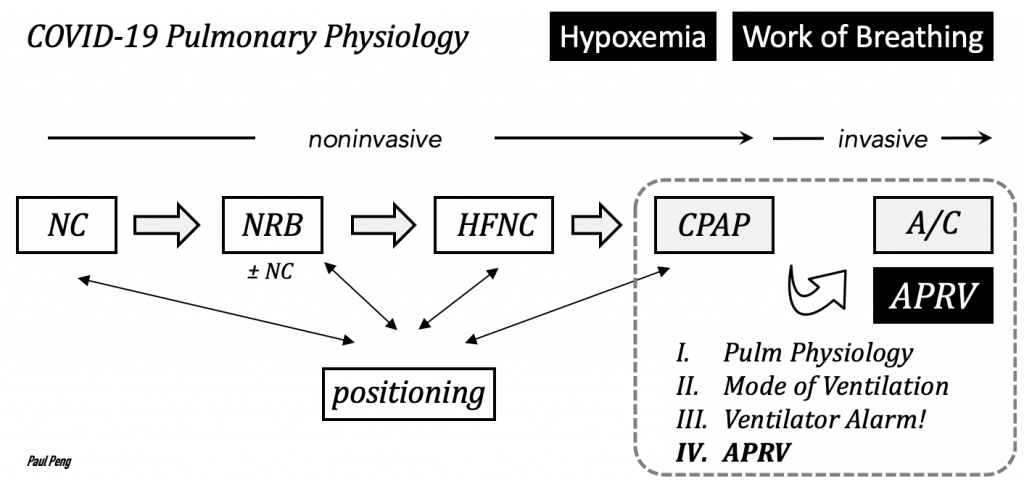
Airway pressure release ventilation (APRV) was used historically as a rescue mode for ARDS, which is classically characterized by heterogeneous lung injury resulting in uneven distribution of ventilation.
The two main theoretical advantages of APRV for intubated COVID patients are:
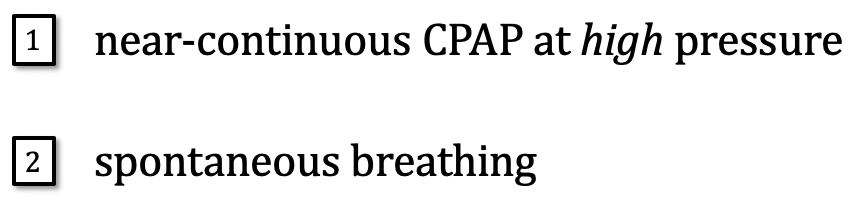
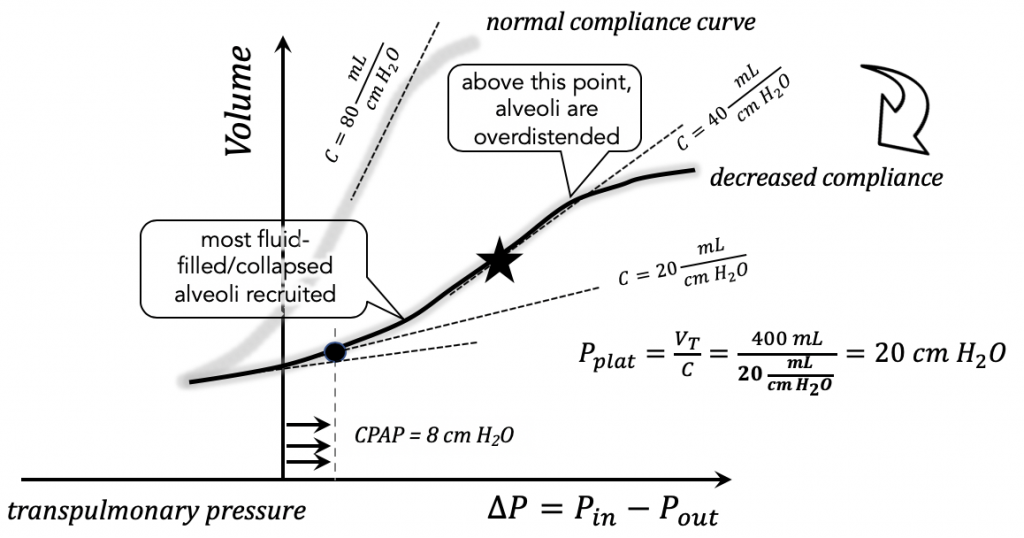
The benefits of CPAP (covered in work of breathing) include shifting to a more compliant region (steeper slope) of the lung-chest wall compliance curve (which helps work of breathing) and for PEEP to reduce shunt.
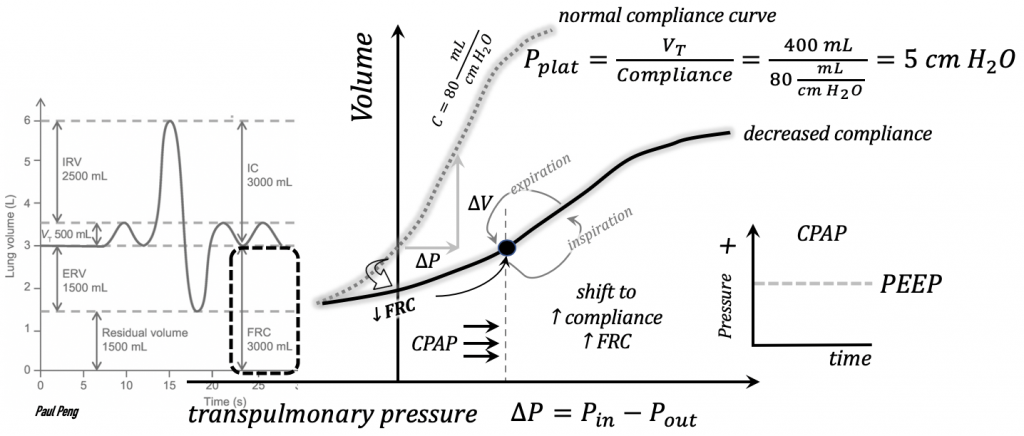
Allowing the moderately-sedated patient to maintain spontaneous breathing is also advantageous for better V/Q matching:
Suppose the COVID patient has progressed to the low-compliance (e.g. C = 20 mL / cm H2O) inflammatory state.
CPAP no longer shifts much along the compliance curve (corresponding to a plateau pressure of 20 cm H2O, assuming VT = 400 mL), and there is increased WOB.
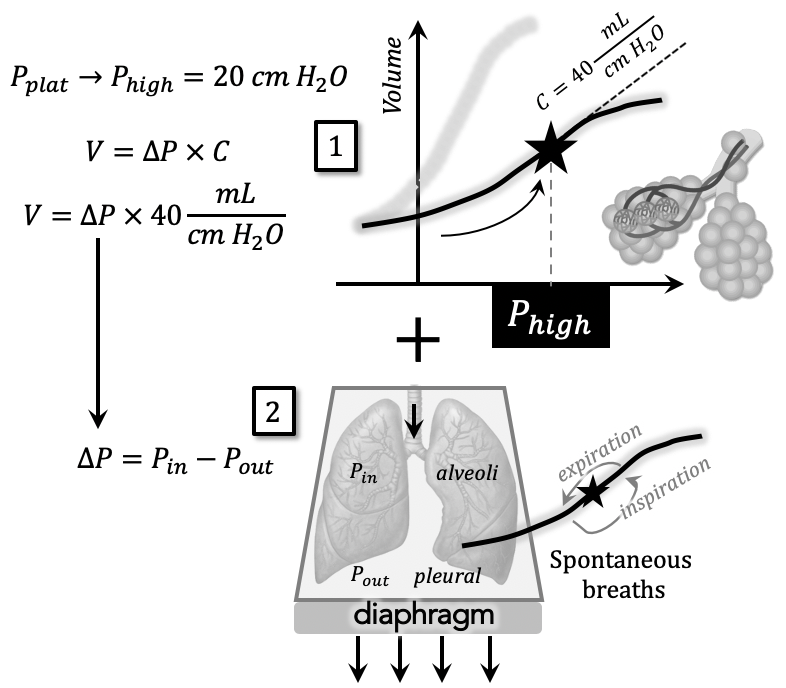
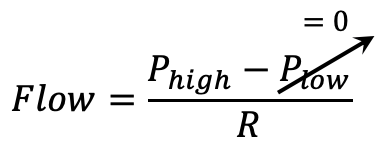
Define Phigh to be the high pressure setting of APRV.
This is empirically set equal to plateau pressure, Pplat = Phigh.
(note that Phigh is not known a priori, but is the theoretical sweet spot of compliance between derecruitment / overdistention. It needs to be titrated while observing oxygenation / ventilation)
Spontaneous breaths are still allowed at this high pressure: a transpulmonary pressure ∆P = 3 cm H2O can generate a VT = (3 cm)(40 mL/cm H2O) = 120 mL.
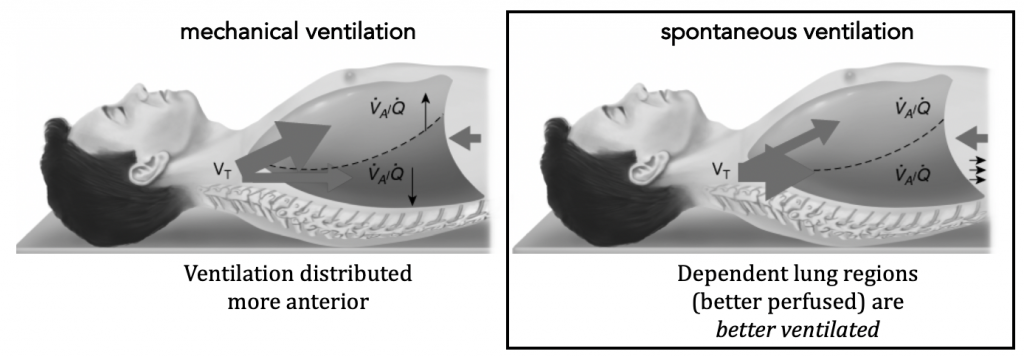
Suppose Phigh is held for time Thigh and is then “released” briefly (i.e. airway pressure release) before returning back to Phigh.
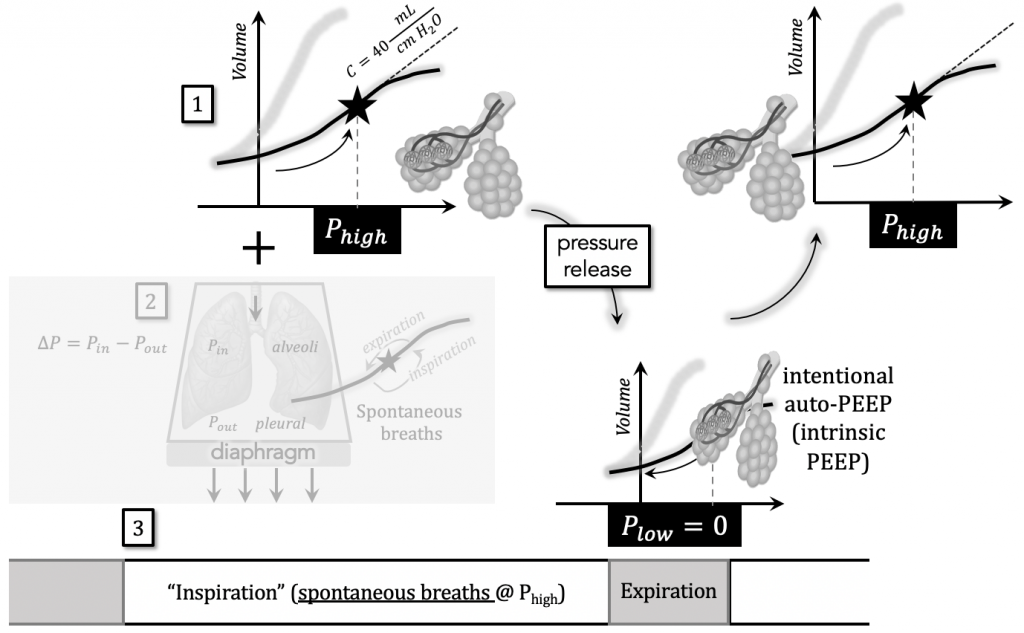
Let “briefly” be defined as time Tlow.
This variable is important to:
- allow the volume of air held during Thigh to be ventilated
- intentionally leave safe levels of auto-PEEP to prevent derecruitment
Plow = 0 in order to maximize the pressure gradient during the brief release period Tlow for maximal ventilation.
Attention needs to be paid to the end-inspiratory volumes (overdistention) generated by the patient as these can lead to microvascular lung injury (volutrauma).
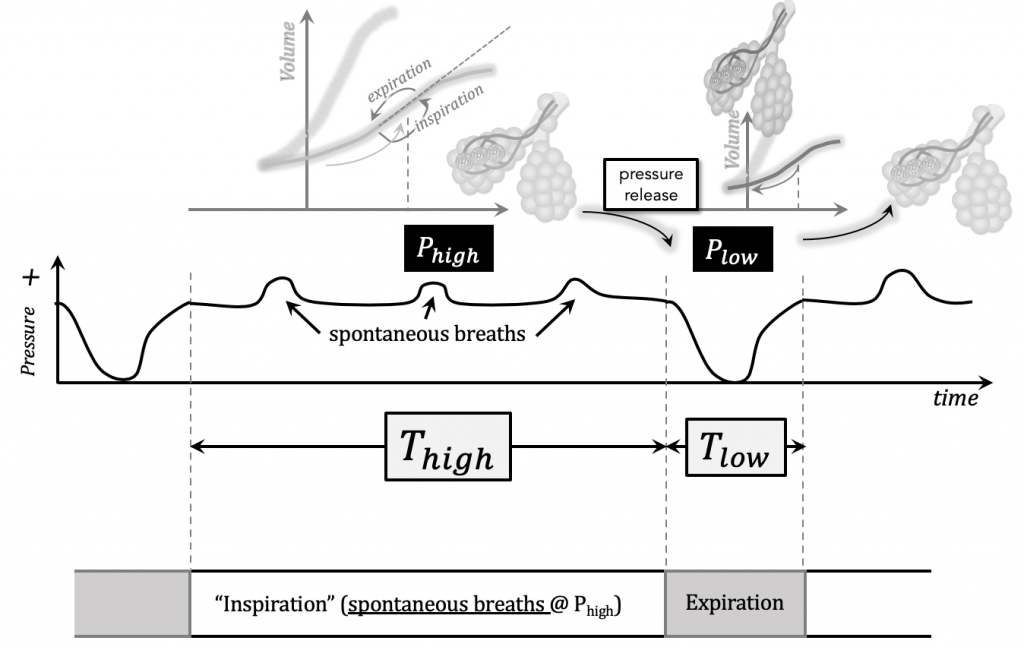
In summary, near-continuous CPAP at Phigh (i.e. high mean airway pressures) is achieved while allowing spontaneous breaths and mandatory ventilation at the release frequency.
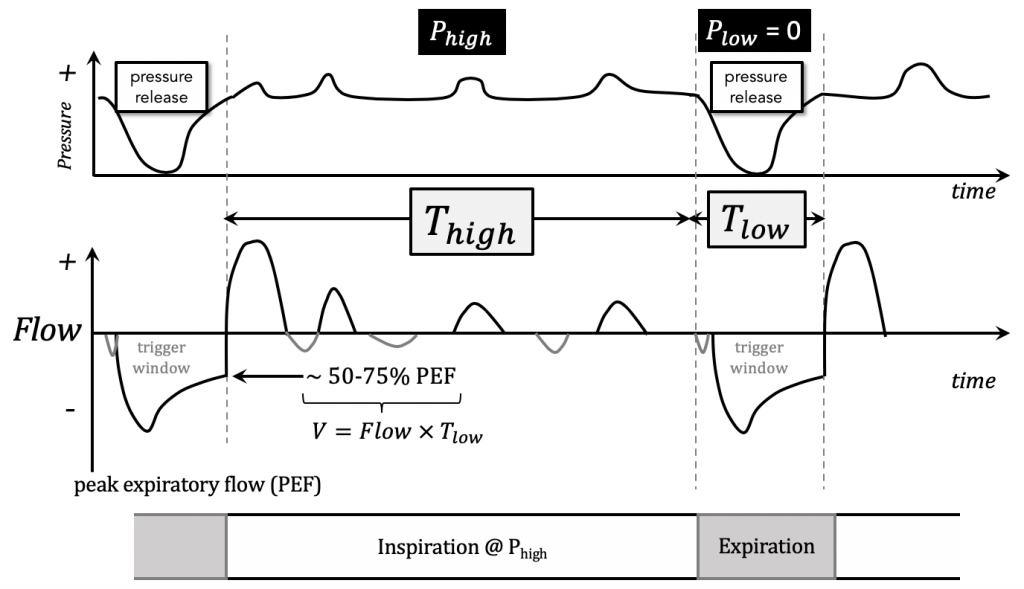
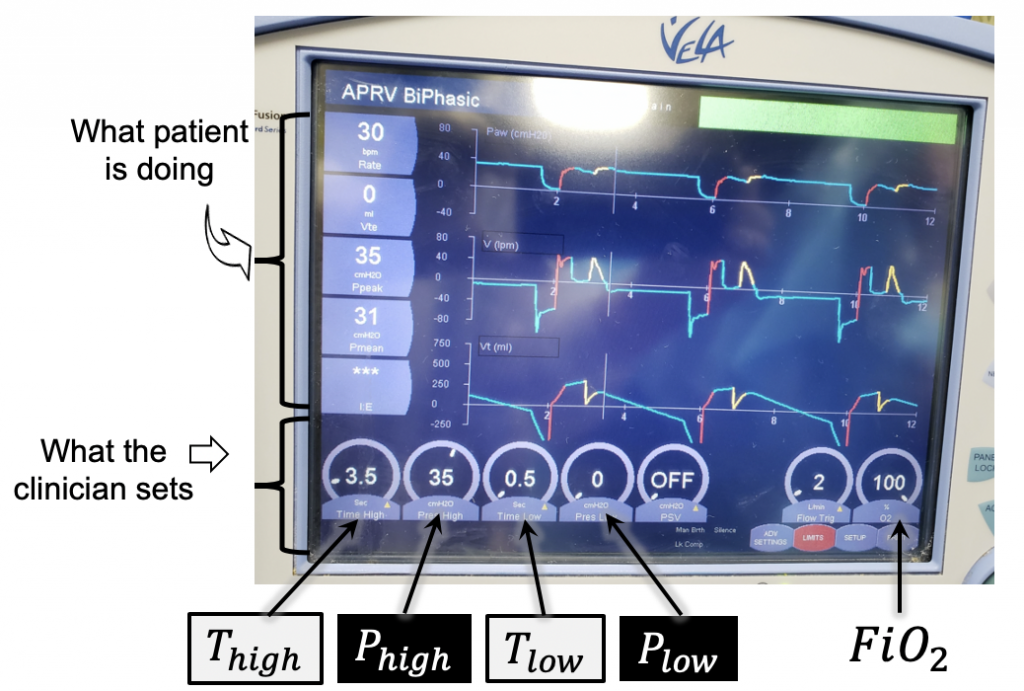
Because the clinician sets the the time trigger and cycle, one breath cycle is equal to a total time, T = Thigh + Tlow , and the inverse of this is the mandatory respiratory rate (RR).
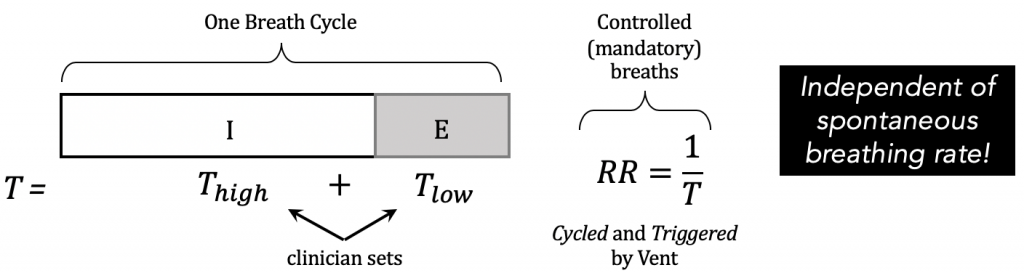
RR is also known as the pressure release frequency, which can be titrated for hyper/hypo-carbia if the patient is not breathing spontaneously.
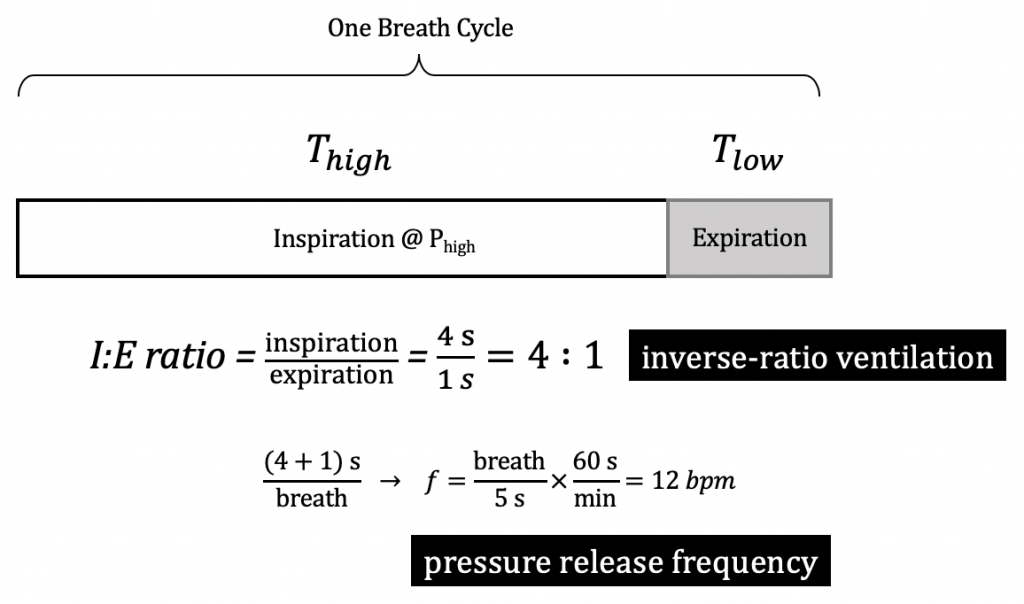
Inverse-ratio ventilation was also used as rescue mode of ventilation to moderate-severe ARDS, but failed to demonstrate significant improvement in mortality when compared to conventional modes.
Implementation
- Set starting pressure parameters: Phigh = Pplat (initial guess of sweet spot of compliance curve), Plow = 0.
- Set starting time parameters: if the patient is not breathing spontaneously, Thigh = 1.7 and Tlow = 0.3 would yield a total T = 2 seconds/breath and a mandatory RR = 1/T = 30 breaths/min. Increase Thigh if inspiratory efforts present.
- Examine Flow-time curve. Tweak Tlow such that expiratory phase stops 50-75% of peak expiratory flow rate (intentional auto-PEEP).
- Set FiO2 initially to 100%, titrate downward to SpO2 target 90-96%. May need to change Phigh as needed.
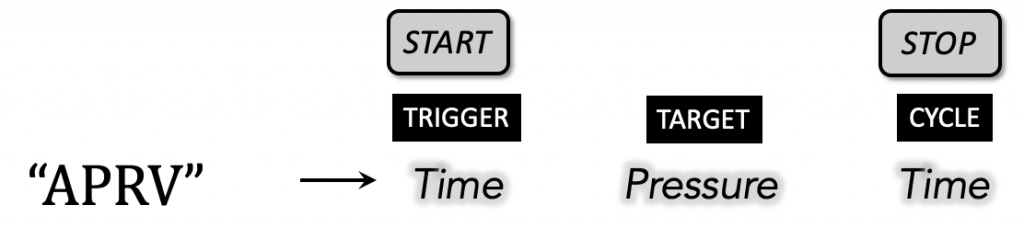
Recall the phase variables characterizing a mode of ventilation; for example, assist/control flow-targeted, volume-cycled (a.k.a. volume-controlled):

In APRV, spontaneous demand breaths are triggered at the two alternating baseline pressure levels and cycled by time:
APRV in action, titrated to SpO2 90%. This patient was previously on A/C-VC 24 | 530 | 100% | 15 with a Pplat = 30 cm H2O.
Note: (optional) A pressure support (PSV) of 8 cm H2O was added to overcome work from resistive circuit during spontaneous breaths.
