He dribbles calmly at the top of the key. Fakes right, crossover, drives forward, spin move. 2 ankles down, 0 to go. He takes a step and finishes with a huge dunk. Boom, right shoulder comes out.
…Alright, so this never happened, but I wanted you to open this article about a technique for anterior shoulder dislocation reduction that requires NO anesthesia/sedation.
My disclaimer is that this is in no way meant to be a comprehensive or superior email about shoulder reductions, it’s simply another technique to add to your repertoire with a pretty interesting premise. As many of you go through residency you will develop your preferred technique, which you will master and teach to your own students, but every once in a while, something comes along that really makes you reconsider if you should change your practice.
At its core, anterior shoulder dislocations are pretty straightforward and common. Nonetheless, there are a few key points that you should consider including but not limited to:
- Is this a recurrent vs first time dislocation?
- Is there trauma/what was the mechanism?
- Is there presence of a fracture/should there be pre-reduction imaging?
- Is the extremity neurovascularly intact?
All this aside, you have determined this is an anterior shoulder dislocation. And maybe you’re feeling particularly bold that day and you want to try a new technique. I want to advocate for this one. (btw, luxation = dislocation, when you’re European)
Title: Reduction of Acute Shoulder Dislocations in a Remote Environment: A Prospective Multicenter Observational Study (2015)
Objective: Present a novel technique for shoulder relocation that can be done in remote environments without medication, adjuncts, and assistants and is well tolerated by patients
Methods:
- Prospective observational study over a 5 year period (2009-2013), in mountains of France/Germany
- Inclusion criteria for the study were: 1) age 16 years or older; 2) ability to give consent; 3) first-time dislocations; 4) no other life-threatening injuries; and 5) repositioning maneuver performed by 1 of our 3 mountain medicine physicians.
- The exclusion criteria included: 1) prior sedation or analgesia; 2) dislocation obviously associated with fractures; 3) mental confusion; 4) refusal to consent; 5) presentation of the dislocation more than 12 hours after event; and 6) association with other traumatic injuries.
- Dislocation was confirmed by 1 of 3 certified wilderness physicians clinically (no imaging)
- Successful reduction was determined by clinical signs and symptoms, including absence of pain, full recovery of range of motion, and normal appearance of the shoulder. Neurovascular examinations were performed before and after reduction.
- No anesthesia, sedation, or joint injection was used!
- Post reduction survey was done to assess patient pain/comfort
- 2 week follow up XR was done to r/o other shoulder injuries
Reduction Technique (watch the video, it’s short!)
- Hold the patient’s wrist with the same hand as the injuried shoulder (left shoulder dislocation, hold the pt’s wrist with your left hand) and the pt’s elbow with the your othe rhand
- Flex the pt’s elbow to 90 degrees and raise the pt’s humerus forward to 90 degrees
- While keeping the shoulder flexed foward at 90 degrees, adducted the glenohumeral joint until the pt’s elbow reaches the midline of the body
- Keeping the elbow at midline, internally rotate the shoulder. Apply constant internal rotation pressure to overcome the MILD resistance met at ~25-30 degrees of rotation WITHOUT pain.
- Continue applying pressure until reduction is achieved at ~30 degrees of internal rotation.
Results
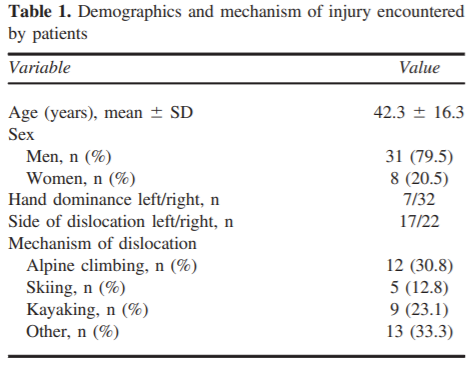
- Successful Reduction was achieved 100% with a maximum of 2 attempts (determined clinically)
- Reduction time averaged about 6.4 minutes (Read: this was done very slowly)
- Time from injury to reduction was about 4 +/- 2 hours
- VAS pain scale score was about 1.7 +/- 1.4 (WOW!)
- No complications
Discussion/Limitations
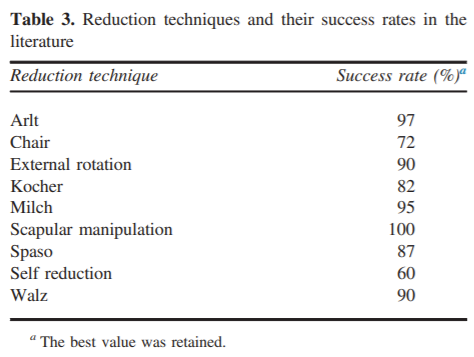
- In the literature, many techniques are also highly successful!
- This is an OBSERVATIONAL STUDY…this is not powered to give results
- This technique was NOT compared to another technique, therefore cannot determine superiority
- This technique was only done by physicians (specialty not determined)
Anecdotal Experience (read: lowest level of data, similar to urban legend)…Since learning this technique, I have successfully done it 2 out of 4 times with only intra-articular joint injection. 1 out of 4 times without any anesthesia. 1 out of 4 times I reflexed to traction/counter-traction with conscious sedation. This even worked on a patient who stated she was consciously sedated the last 3 times!
The Takeaway: This is yet another technique to add to your arsenal of reduction techniques. The appeal of this technique comes from its ability to be applied in remote conditions without anesthesia or sedation or the presence of other hands. The study technique is not able to determine if this is superior to other techniques.
