As alluded to in the first post, don’t be fooled by a “normal” potassium in the setting of DKA because osmotic diuresis and H+/K+ exchange means that total body potassium is actually LOW.
You all know this, but don’t forget to check the potassium before starting insulin. 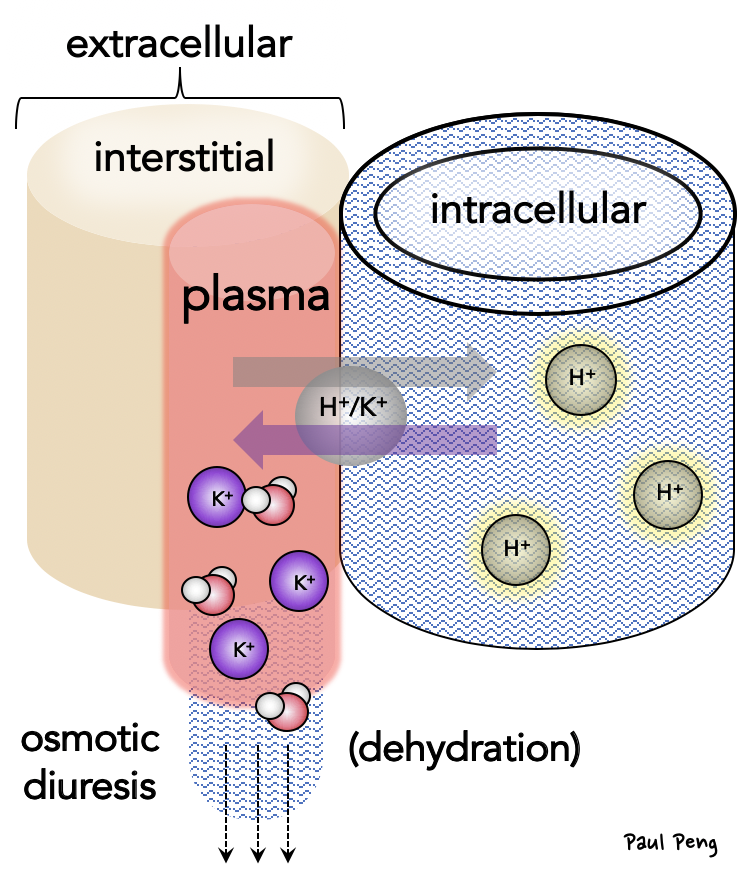 But what about the acidemia? How does that affect physiology?
But what about the acidemia? How does that affect physiology?
(reminder: use acidosis to describe the process of increasing [H+]; acidemia is the state of increased [H+] measured in blood)
At the cellular level, acidemia is likely denaturing critical proteins leading to the physiologic dysfunction.
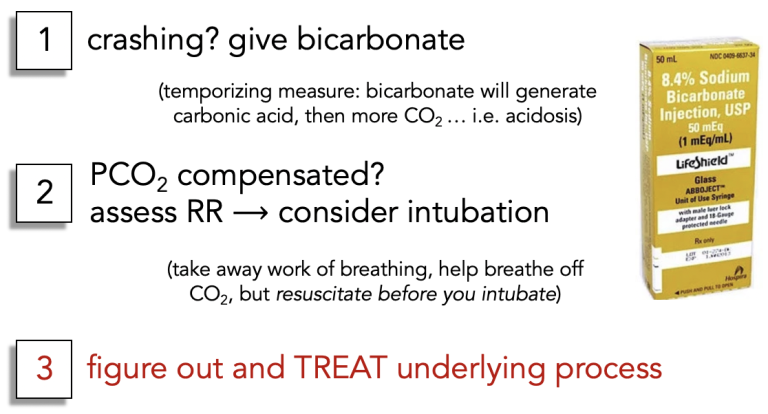
What are the immediate Resus goals if you encounter acidemia?
 Possible future post: acid-base compensation, Resus acidosis physiology (e.g. DKA, severe asthma, etc.)
Possible future post: acid-base compensation, Resus acidosis physiology (e.g. DKA, severe asthma, etc.)
Overall, the key step is to identify and reverse the origin of the acid disturbance!
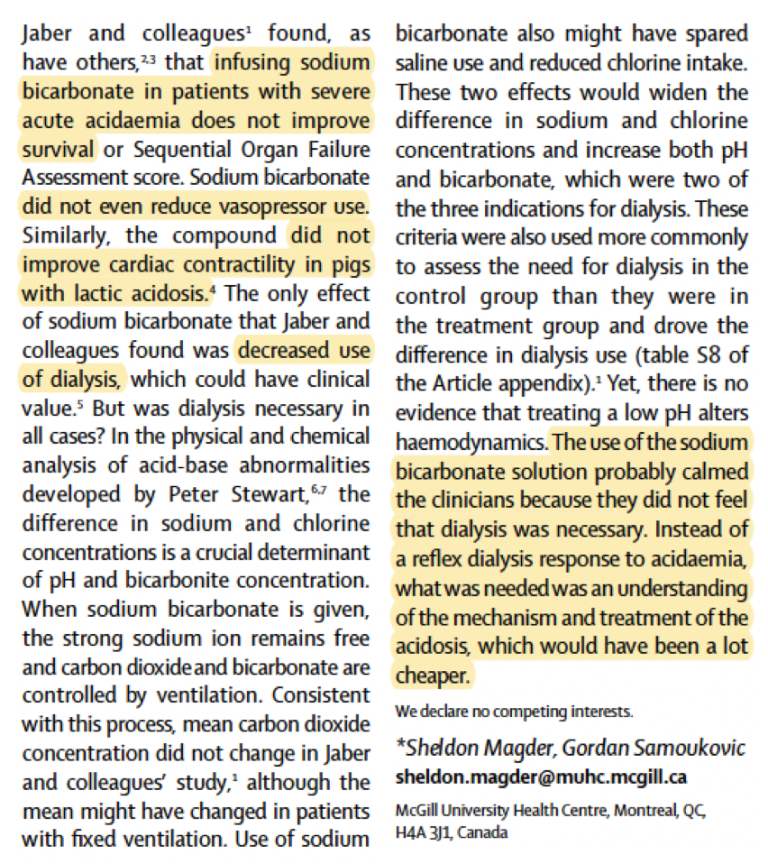
If you have gotten down this far, then you may have heard of the BICAR-ICU trial investigating the efficacy of bicarbonate infusions in ICU patients with severe metabolic acidemia. It is worth reading a comment on this trial by the legendary Sheldon Magder, reproduced below: