Septic Shock and you want me to give Esmolol?
Written by Erena Weathers
Today’s pearl is a fun one, and one it seems not many have heard about. It is the idea in septic shock you can give esmolol to improve mortality.
“But Erena, we need pressors in shock and now you’re telling me we are going to use a beta-blocker in someone who is in shock?”Yes, because septic shock myopathy exists due to high amounts of catecholamines, and esmolol can help prevent that. Patients with tachycardia suffer from increased myocardial oxygen demand and cardiac load, reduced ventricular diastolic time, and subsequently insufficient coronary perfusion.
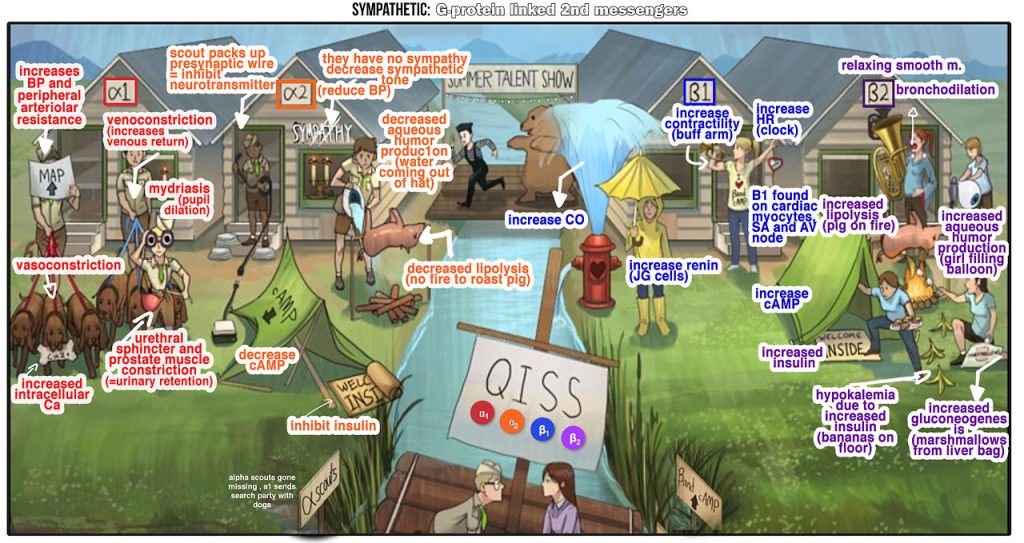
But first, let’s review. Esmolol is a cardio-selective beta-blocker meaning it predominately targets B-1 receptors on the heart. It is also a very fast “on and off” drug with a rapid distribution half-life of about 2 minutes and an elimination half-life of about 9 minutes. This means if you try this and the pressure starts to go down, you can quickly turn off the drip and all is well.
Here’s a quick review of alpha and beta receptor effects:
Now that we have that settled and a little Step 1 review done, let’s get to the fun part. I volunteered to write up ResusX summaries, and one of the topics was about “Last Line Pressors” and esmolol was brought up. I thought this was interesting, and then it kind of fell out of my brain. Earlier this week, Dr. Devivo gave a nice pressor talk while in Resus and we got to talking about esmolol and I thought I should make a pearl.
So the idea is you have a relatively “healthy” septic patient. You have given appropriate fluids and started levophed. The patient is sitting at 20 of levo, and tachycardic to 130s-140s, and you’re toying with the idea of adding on vaso or another pressor. In this case, I would echo the heart to see if the patient isn’t in concomitant cardiogenic shock (in that case the persistent tachycardia is probably compensatory). If that isn’t the case, you have a patient who has been resuscitated and the high amount of catecholamines is causing damage to the heart and other organs, and the tachycardia is not allowing for proper filling of the ventricle and perfusion of the heart, so slowing down the heart would be ideal. This is where esmolol comes in. You would start an esmolol gtt 25-50 and titrate to a HR 80-95ish.
Morelli, Andrea, et al. “Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial.” JAMA 310.16 (2013): 1683-1691.
This was a randomized phase II trial in Spain of 77 patients in the ICU receiving esmolol and 77 controls receiving standard treatment. Twenty-eight day mortality was 49.4% in the esmolol group vs 80.5% in the control group (adjusted hazard ratio, 0.39; 95% CI, 0.26 to 0.59; P < .001). For patients in septic shock, open-label use of esmolol vs standard care was associated with reductions in heart rates to achieve target levels, without increased adverse events.
Brown, Samuel M., et al. “Esmolol infusion in patients with septic shock and tachycardia: a prospective, single-arm, feasibility study.” Pilot and feasibility studies 4.1 (2018): 1-9.
First in the US, similar to above, but even smaller with only seven patients. Not much gained except that it was safe.
Liu, Ping, et al. “The influence of esmolol on septic shock and sepsis: A meta-analysis of randomized controlled studies.” The American Journal of Emergency Medicine. 36.3 (2018): 470-474.
5 studies were included in this analysis, and the treatment of esmolol was associated with decreased 28-day mortality (RR 0.66, 95% CI 0.56–0.77, p < 0.001) with no heterogeneity among the studies (I2 0%, heterogeneity P 0.46). The five studies are published between 2013 and 2015, and sample sizes range from 41 to 154. Esmolol intervention shows no remarkable influence on MAP (Std. MD 0.11; 95% CI − 0.21 to 0.44; P 0.49 and CVP (Std. MD − 0.11; 95% CI − 0.50 to 0.28; P 0.58), but can significantly reduce heart rate (Std. MD − 2.43; 95% CI − 4.13 to − 0.72; P 0.005).
Hasegawa, Daisuke, et al. “Effect of Ultrashort-Acting β-Blockers on Mortality in Patients With Sepsis With Persistent Tachycardia Despite Initial Resuscitation: A Systematic Review and Meta-analysis of Randomized Controlled Trials.” Chest (2021) 159(6):2289-2300.
This was a systematic review of 7 RCTs, 613 patients, with sepsis and persistent tachycardia after initial resuscitation who received either esmolol or landiolol. Six trials (572 patients) were meta-analyzed for the outcome of 28-day mortality. Mortality risk was reduced by 32% in patients who received a β-blocker vs placebo (RR 0.68; 95% CI 0.54 – 0.85). Overall mortality rate was 36.7% in the esmolol/landiolol cohort, 54.9% in the placebo group; absolute risk reduction 18.2%, NNT 5.5. Heterogeneity was low (I2 31%).
Huang, Po, et al. “The Efficacy and Safety of Esmolol for Septic Shock: A Systematic Review and Meta-analysis of Randomized Controlled Trials.” Frontiers in pharmacology 12 (2021): 1318.
Fourteen studies with 927 participants were included. The primary outcome is 28-day mortality with nine studies with 708 participants reported 28-day mortality. The result showed that 28-day mortality is lower in the esmolol group than in the control group (RR 0.66, 95% CI 0.56-0.77, p < 0.01). There was obvious heterogeneity among these included studies and indicated that esmolol plus standard treatment could decrease HR when compared with standard therapy. The meta-analysis of nine studies showed that compared with standard therapy, adding esmolol has no influence on MAP at 72h. Three studies reported adverse events and there was no significant difference in the adverse effects among the two groups.
Erena’s takeaway: When I have a septic patient I know I have fluid resuscitated but who is sitting there with tachycardia, I will think about esmolol. I will echo the heart and look for signs of cardiac failure. If there are no signs of heart failure, and the patient has persistent tachycardia and is adequately fluid resuscitated, on a pressor, I will start an esmolol gtt at 25. Devivo said 50, but I haven’t done this and from discussion, this isn’t done much downstairs but done more upstairs. But as Leibner likes to say, we should be giving upstairs care downstairs.
References
SketchyPharmacy. “Sympathetic Drugs: G-Protein Linked 2nd Messengers.” Sketchy Group LLC.
Morelli, Andrea, et al. “Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial.” JAMA. 310.16 (2013): 1683-1691.
Brown, Samuel M., et al. “Esmolol infusion in patients with septic shock and tachycardia: a prospective, single-arm, feasibility study.” Pilot and Feasibility Studies. 4.1 (2018): 1-9.
Liu, Ping, et al. “The influence of esmolol on septic shock and sepsis: A meta-analysis of randomized controlled studies.” The American Journal of Emergency Medicine .36.3 (2018): 470-474.
Hasegawa, Daisuke, et al. “Effect of Ultrashort-Acting β-Blockers on Mortality in Patients With Sepsis With Persistent Tachycardia Despite Initial Resuscitation: A Systematic Review and Meta-analysis of Randomized Controlled Trials.” Chest. (2021) 159(6):2289-2300.
Huang, Po, et al. “The Efficacy and Safety of Esmolol for Septic Shock: A Systematic Review and Meta-analysis of Randomized Controlled Trials.” Frontiers in Pharmacology. 12 (2021): 1318.
