(Previous posts: mode of ventilation, work of breathing)
As the ventilator alarm grows louder and louder as you walk closer to the room of the patient you just intubated, you review the “DOPES” mnemonic in your head. Except that in the COVID era, you have to be careful with aerosolization (can’t BVM or allow ETT open to air).
To review some critical actions:
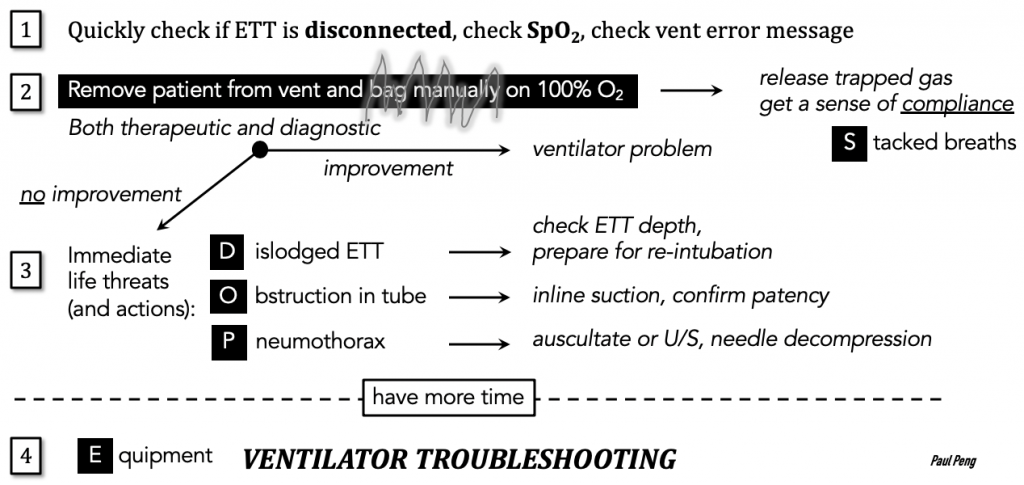
Next, confirm that there is adequate post-intubation analgesia and sedation.
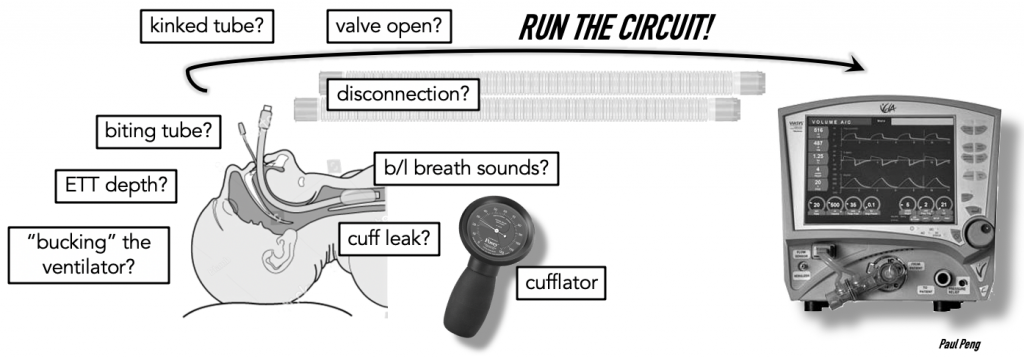
Then, my approach is to systematically “run the tube” from beginning (ETT) to end (ventilator).
Any leak, either from the deflated cuff or an opened valve, can cause a low tidal volume alarm.
The Pressure Alarm
Consequence of a pressure alarm:
Vent will stop delivering flow! Patient receives low VT!
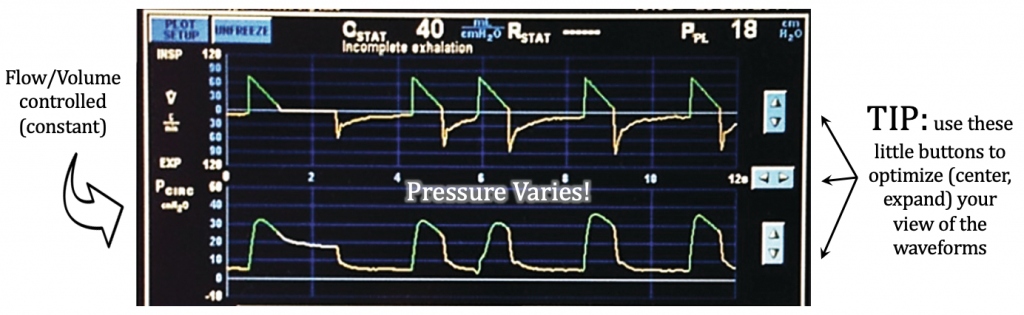
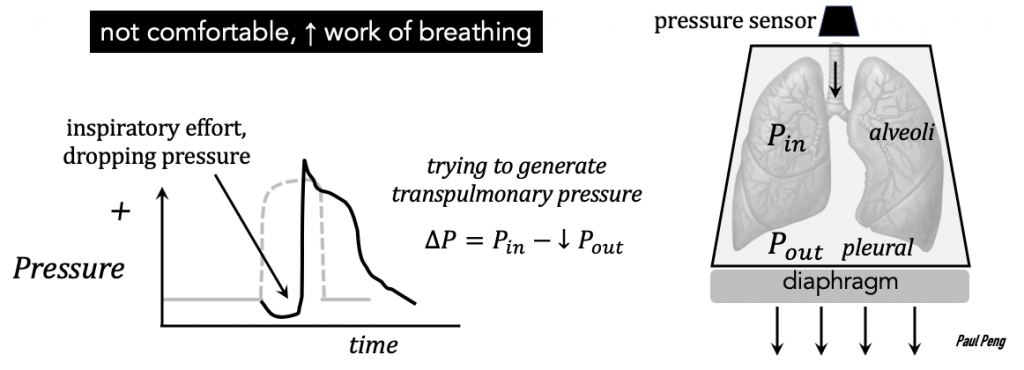
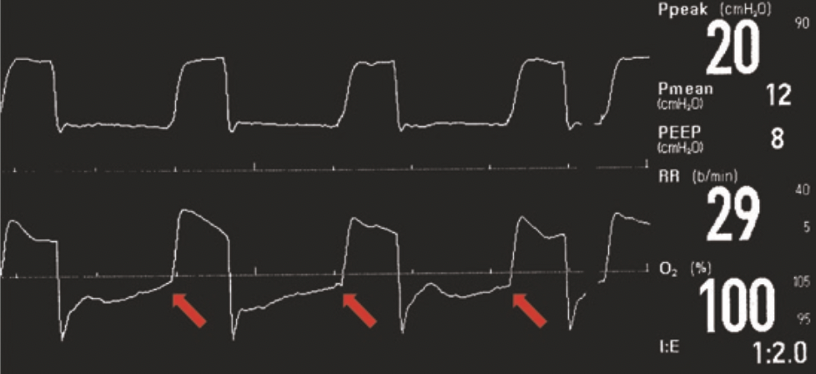
Hone in on the pressure-time curve on the ventilator because volume-control means pressure-varies; and the latter will contain useful information.
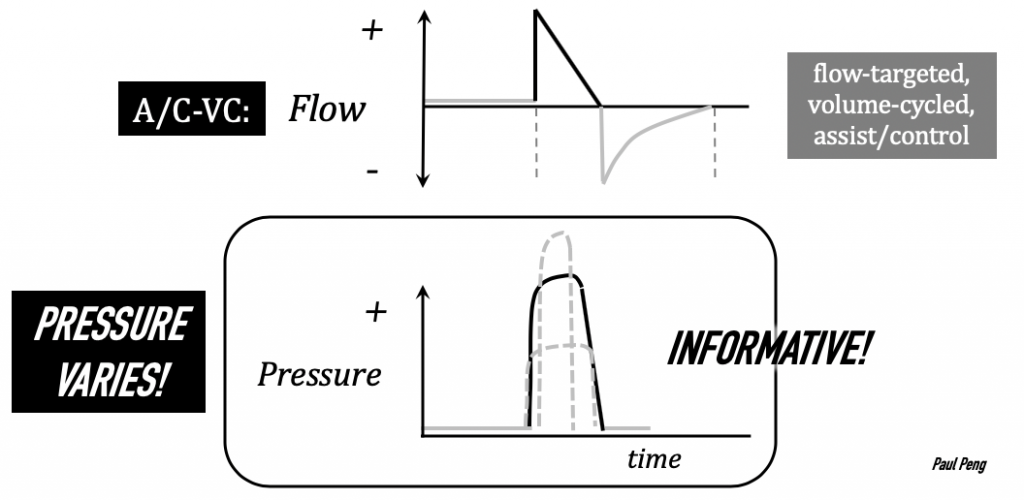
For instance, a patient in respiratory distress often tries taking deeper breaths (think about the large transpulmonary pressures needed to generate a sufficient tidal volume). If this inspiratory effort is not matched with what the ventilator is delivering, then the pressure-time curve would look scooped-out.
A very common alarm encountered is high peak airway pressures.
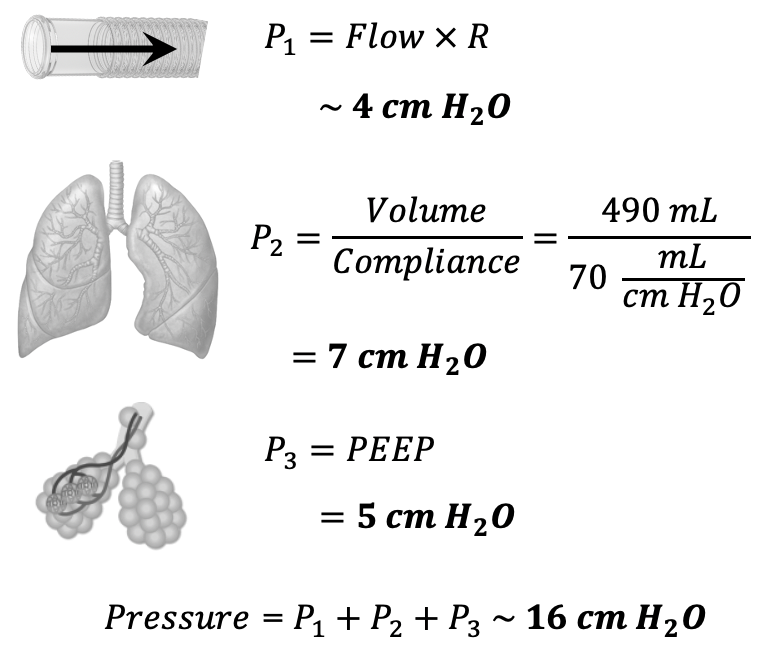
Airway pressure only has 3 components.
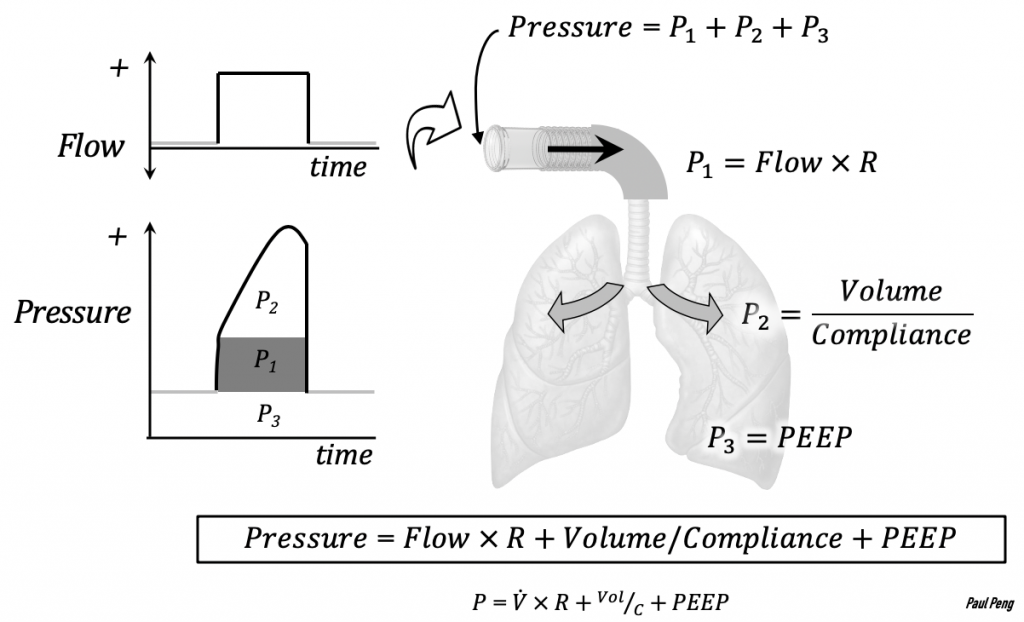
Consequently, we can break down the differential diagnoses of each pressure component systematically:
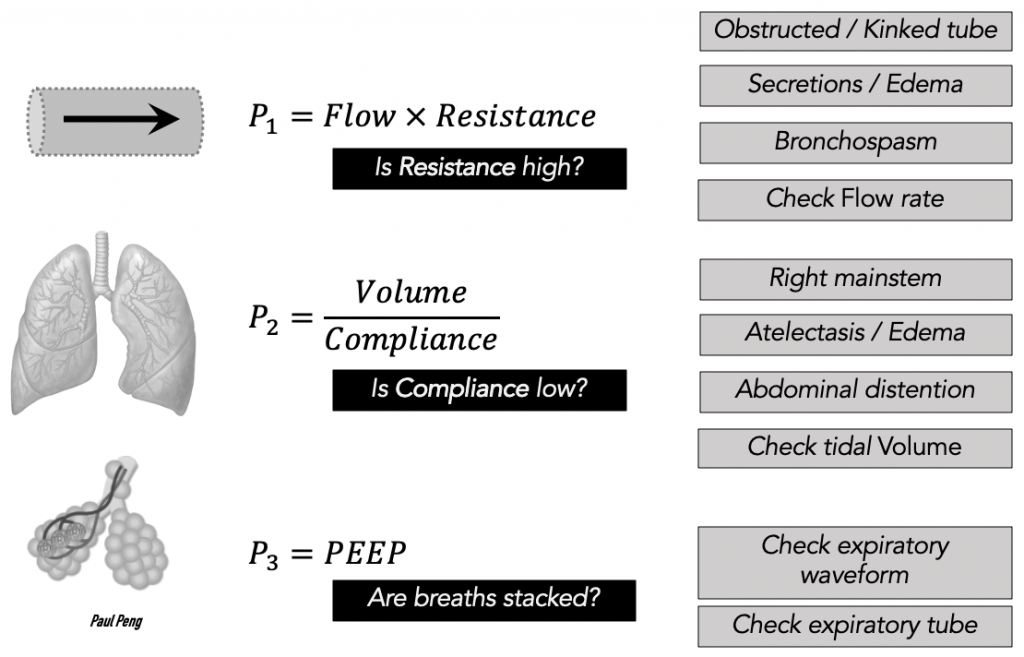
P1
Bring an inline suction to bedside and examine each piece of the circuit (i.e. run the tube). Note any grimacing or biting, indicating insufficient analgesia/sedation.
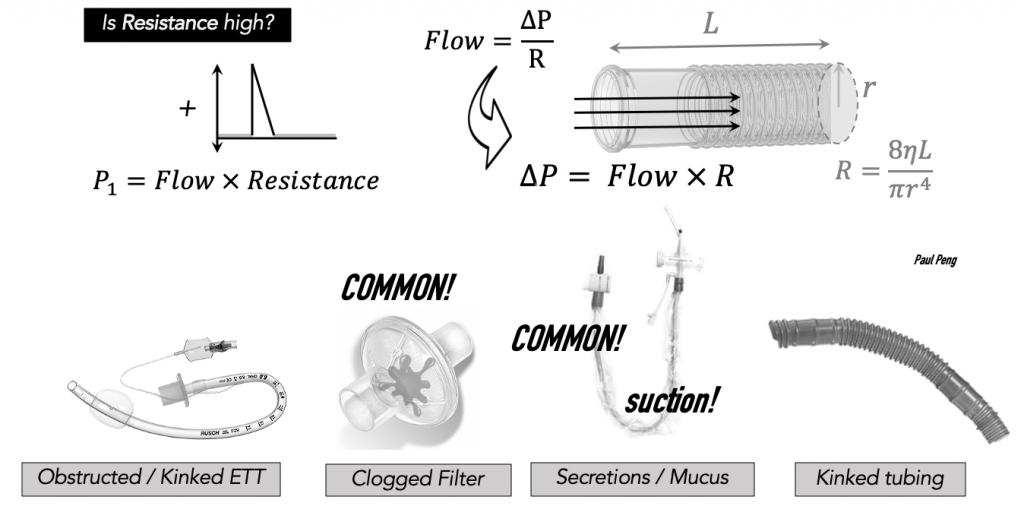
!! If you are going to swap out a clogged filter: wrap the ETT with gauze (to protect it from being damaged), clamp the tube with a kelly clamp, and then remove the filter, to prevent aerosolization !!
P2
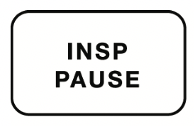
The key maneuver for separating out the rest of the etiologies of high peak pressures is the inspiratory pause/hold. Note: this is only in the setting of invasive ventilation such as A/C-VC mode.
Pressing this button once will initiate an automatic ventilator seal of the breathing circuit for 0.5 to 2 seconds (max) to stabilize a pressure measurement. It will not harm the patient. (It’s possible to press and hold the button for a manual pause (maybe a stabler pressure reading), and this aborts after 7 seconds (not recommended).
Purpose: differentiate if the high pressure is a compliance or resistance issue by taking flow out of the equation.
Now the airway pressure is looking only at the pressure of the lung/alevoli system (assuming PEEP = 0), otherwise known as the plateau pressure, Pplat:
Pplat = tidal volume / compliance
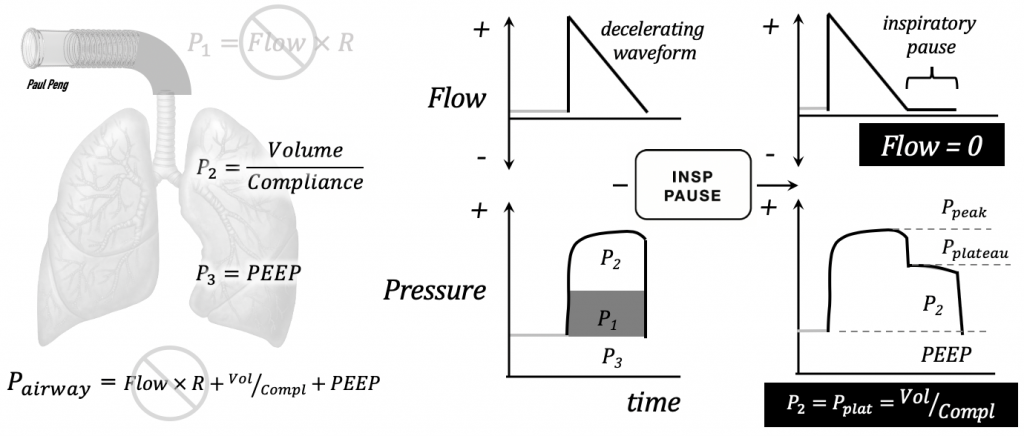
- High Pplat means that compliance is LOW — a lung problem (e.g. atelectasis).
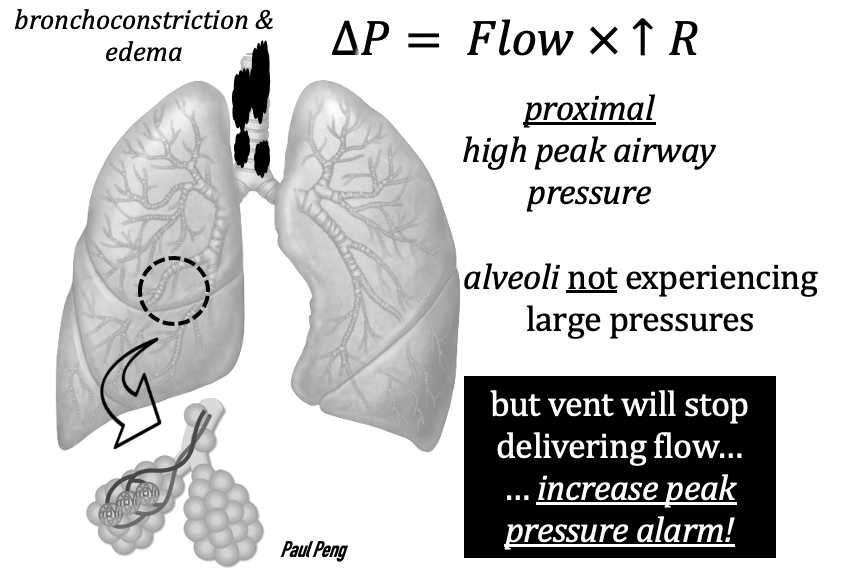
- Low Pplat means there’s a resistance component in the circuit (e.g. bronchoconstriction/edema in COPD/asthma).
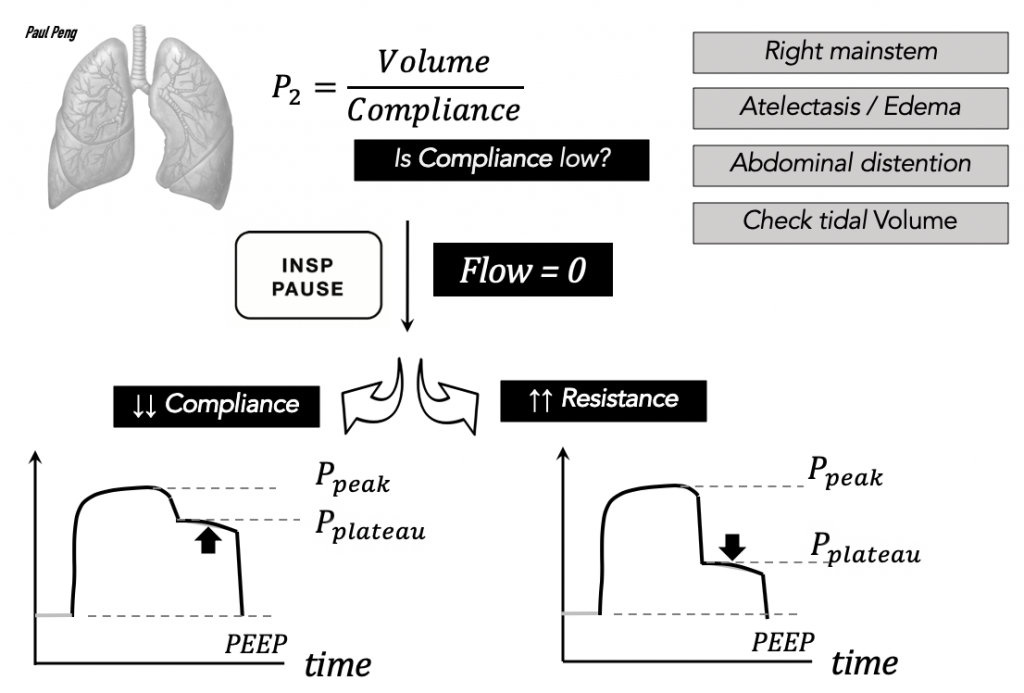
The example above has a relatively low compliance (i.e. lungs not easily stretched) and a Pplat < 30 cm H2O (i.e. lung-protective).
For a more in-depth discussion of Pplat, compliance, read about driving pressure & stress index by Jon-Emile Kenny (or anything on heart-lung!).
Common values for the 3 pressures are:
A brief aside on high peak airway pressures common in an intubated asthma patient: it does not necessarily mean that you are causing barotrauma because the high pressures arise from reduced radius of bronchioles secondary to edema and bronchoconstriction of smooth muscle — only present before the small airways and alveoli.
P3
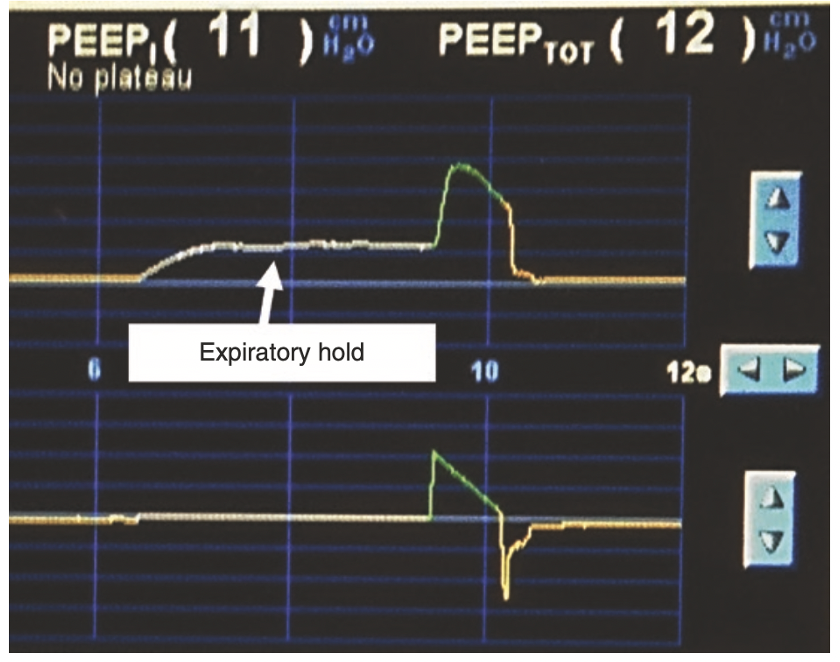
The last component of PEEP is more of a problem if there is underlying obstructive lung pathophysiology:
- COPD/emphysema: small airways collapse on expiration, leaving trapped air
- Asthma: overbreathing, not fully exhaling because of bronchoconstriction
In this case, the flow-time curve is informative: on the expiratory tracing below, the red arrows point to flow that does not return to zero.
The residual, not-fully expired air will generate intrinsic PEEP, PEEPI (also known as auto-PEEP).

Measure auto-PEEP by performing an expiratory pause/hold.
In the following example, the set PEEP = 1 cm H2O. On expiratory pause, pause the measured total PEEP = 12 cm H2O, implying that the intrinsic PEEP = 11 cm H2O.
Based on the previous discussion of ventilator parameters, assuming A/C-VC, what should be the corrective action to prevent further breath stacking?
Also, review permissive hypercapnea! For a future post, hopefully.
References
Wilcox S.R., Aydin A., Marcolini E.G. Mechanical Ventilation in Emergency Medicine.
Martin J. Tobin. Principles and Practice of Mechanical Ventilation, 3e
J. M. Cairo. Pilbeam’s Mechanical Ventilation: Physiological and Clinical
Michael G. Levitzky. Pulmonary Physiology, 9e
Jesse Hall. Principles of Critical Care, 4e
Scott D. Weingart. Managing Initial Mechanical Ventilation in the Emergency Department.
