Cardiac pacing as an intervention can be conceptualized as addressing problems in electrophysiological conduction and/or. So, for example, if there is a disruption in the electrical continuity between the atrium and the ventricle, a pacer maybe function by detecting a normal sinus impulse in the atrium (there is typically a right atrial lead connected to the pacer generator) and “transmitting” (a pacer does not actually transmit native impulses–rather, it generates new ones) an appropriately timed impulse to the ventricle, resulting in synchronous contraction–ideally.
To reiterate the main indications: sinus node dysfunction, acquired AV block, chronic bifascicular block, pause dependent ventricular tachycardia (a pacer would prevent a prolonged pause in this case and thereby prevent Vtach), severe congestive heart failure requiring “cardiac resynchronization therapy” (these patients tend to receive biventricular pacers i.e. NOT “dual chamber”.
Pacers are described by a five letter code, the first three of which are the most relevant

A “DDD” pacer describes a device capable of 1) pacing both atrium and ventricle 2) sensing impulses from both atrium and ventricle and 3) triggering a de novo impulse or inhibiting a detected impulse.
A “VOO” pacer describes a device that simply paces the ventricle without receiving any information about native impulses.
Now that we understand how pacers function, it is important to become familiar with their electrocardiographic signatures. “Pacer spikes” should be visible on the standard EKG (maybe not a 3 lead tele strip) and typically indicate impulse generation. A spike before a p-wave indicates atrial pacing which–in isolated sinus node disease i.e. no AV or ventricular dysfunction–should be followed by normal QRS morphology.
A spike before a QRS complex indicates ventricular pacing. Spikes before both the p-wave and QRS complex indicates dual-chamber pacing.
When a single ventricle is paced (as opposed to BiV pacing), the impulse is transmitted usually through a lead implanted in the right ventricular apex. This will manifest on the EKG as a left bundle branch block pattern, naturally. This should make sense: the pacer lead is bypassing the AV-node and bundle of His and stimulating the right ventricular myocardium first, resulting in right ventricular depolarization followed by left ventricular depolarization. This is more-or-less the electrical conduction abnormality that results from an LBBB. If you do not understand why the morphology looks the same, then you ought to review LBBB.
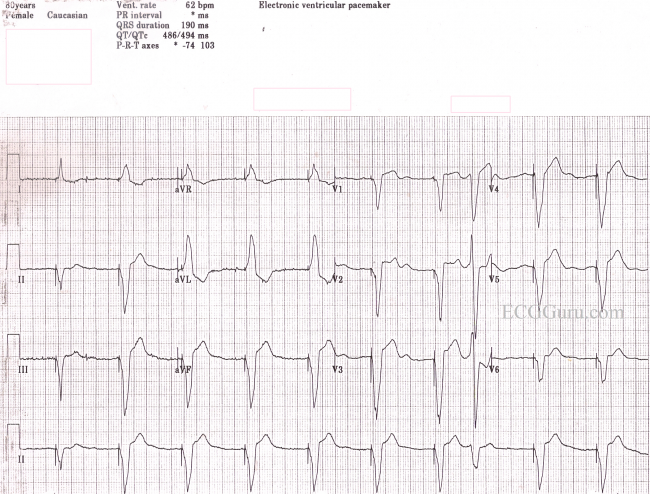
The major difference between an intrinsic LBBB and a paced morphology is the negative QRS in V5-V6 in paced rhythms.
Just as in LBBB, Sgarbossa criteria are useful for detecting ischemia in ventricularly paced rhythms.
