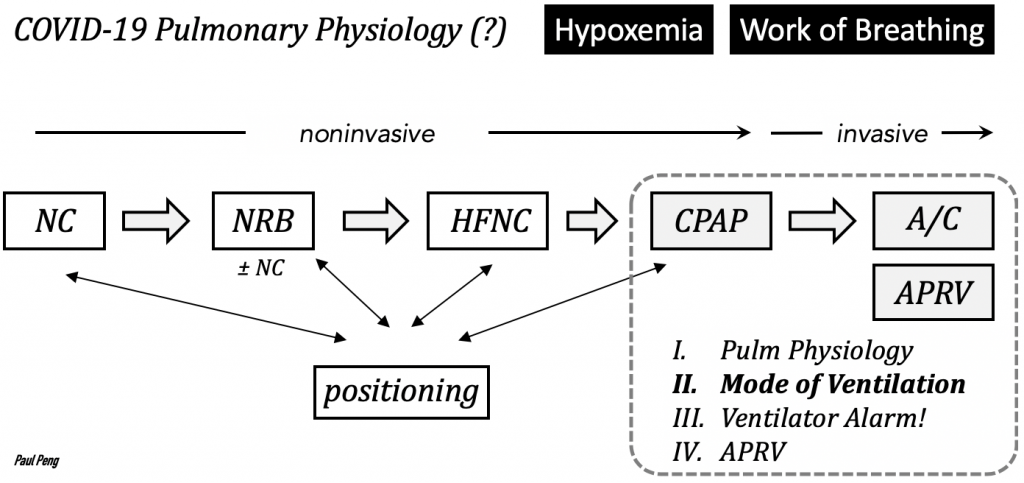
(Previous post reviewed work of breathing, next post: ventilator alarm)
Even though we often place patients on “volume-control ventilation”, the goal of this post is to precisely define the mode of ventilation, which is often inconsistently or loosely described. It will hopefully serve as the foundation for characterizing other advanced modes.
The mode of ventilation consists of the phase variables of a breath: trigger, target, cycle.
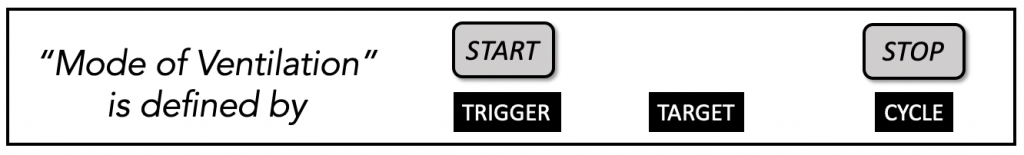
Consider one breath consisting of inspiration and expiration.
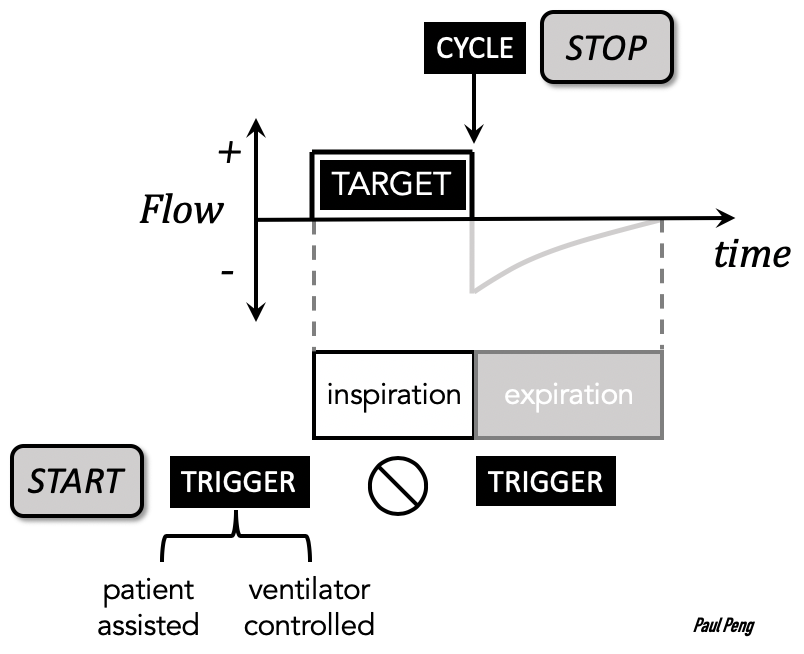
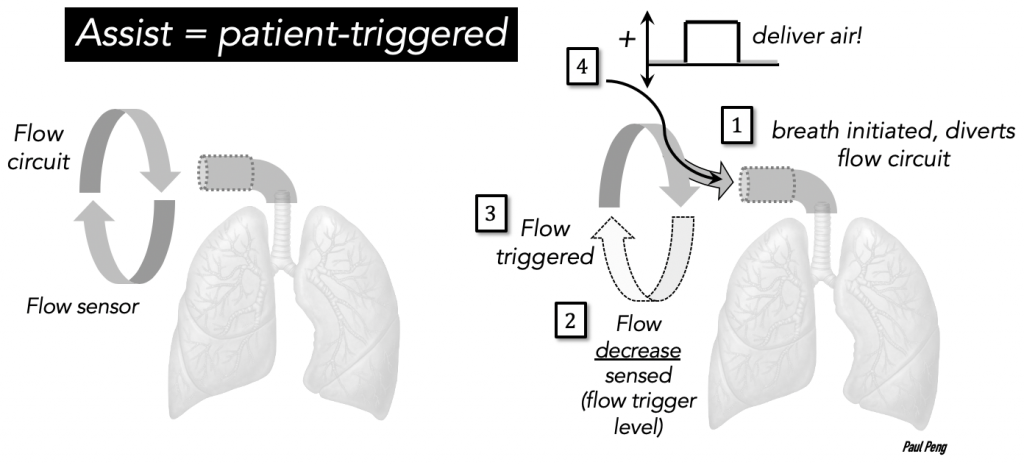
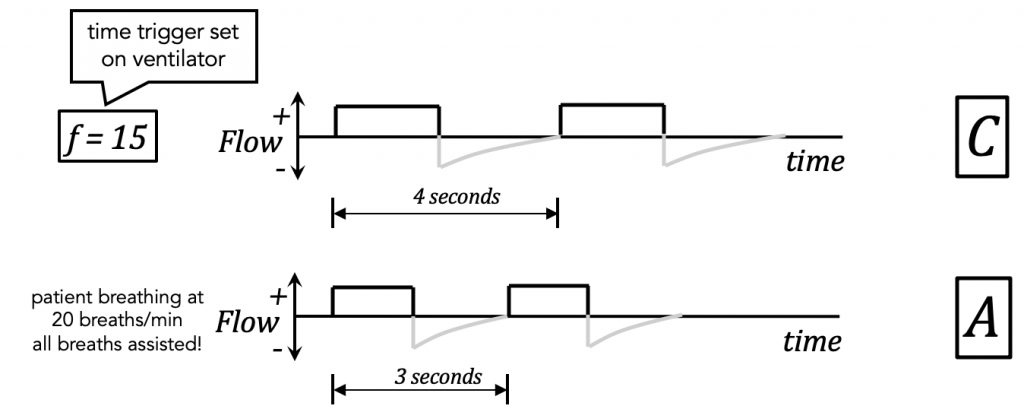
The start of the breath is triggered by the patient or the ventilator. This is what “Assist/Control” means!
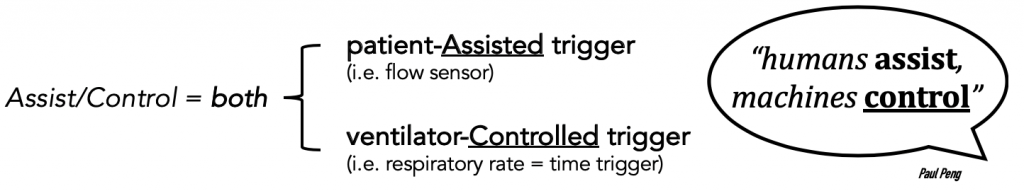
An inspiratory effort by the patient is sensed (only during expiration) as a deflection in flow or pressure (as set by a threshold) and a full volume-cycled assist-breath will be delivered.
- You will see this as an “A” on some ventilators.
- An Assist breath can only be delivered during the phase of expiration.
Pressure support ventilation uses only a patient-assist trigger so it does not deliver time-triggered breaths.
The respiratory rate that you set is basically a time trigger for a ventilator-controlled (a.k.a. mandatory) breath. It will kick in if there’s no inspiratory effort by the patient.
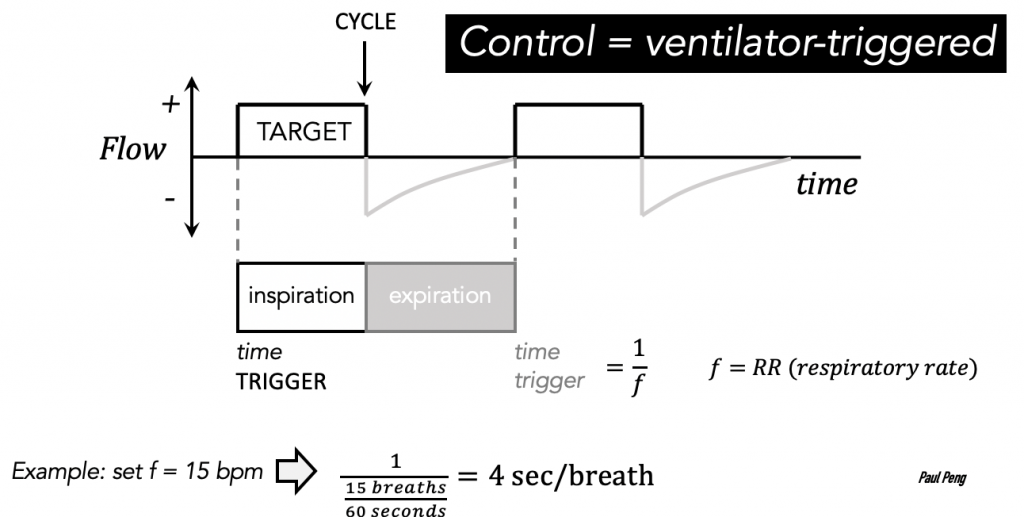
To summarize the Assist/Control trigger:
The target phase variable is regrettably confusing.
When we say “volume-control” or “pressure-control”, we are trying to describe the target.
Unfortunately, there is a lot of inconsistency in the manufacturers’ descriptions as well as in the literature, and target is also known as ‘control’ or ‘limit’.
When we set up for lung-protective ventilation (VT = 6-8 cc/kg) we are not targeting volume directly. Instead, we are selecting a flow-target:
- flow waveform
- flow rate
and cycling (stopping) the flow-target when it reaches our VT.
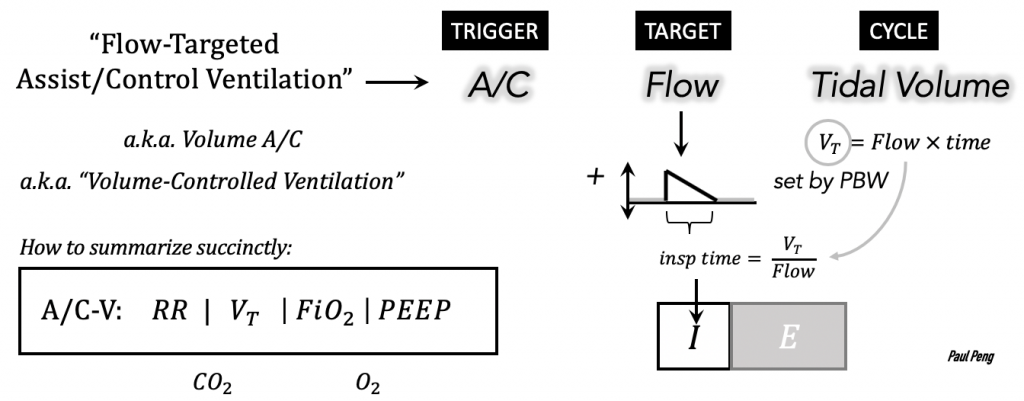
Hence volume-“control” is technically incorrect, but it is so common that it’ll still be used hereafter (but don’t forget that it is flow that is targeted).
Why the two different flow waveforms? Some ventilators only have the default rectangle waveform, but try consciously breathing at a constant flow rate … it is unnatural/uncomfortable! Select the decelerating waveform, if possible, which tries to mimic normal physiology.
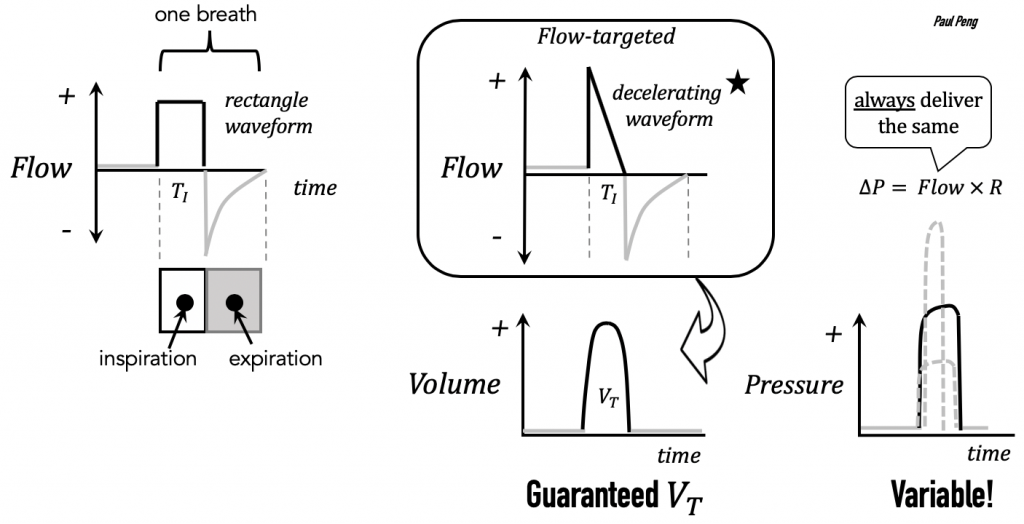
Thus, flow-targeted mechanical ventilation will always deliver the flow target over a period of time to reach the cycle tidal volume, VT.
But note that the pressure-flow equation (P = Flow × R) stipulates that if resistance increases (e.g. mucus secretions, biting endotracheal tube), pressure will increase!
- Key concept: whatever is being controlled (e.g. volume) means the other target (e.g. pressure) varies–A/C-VC means that pressure is allowed to vary
- the target that is varying contains useful information about the vent-patient interaction
Some COVID patients have better vent synchrony while on pressure-targeted ventilation. Why would that be?
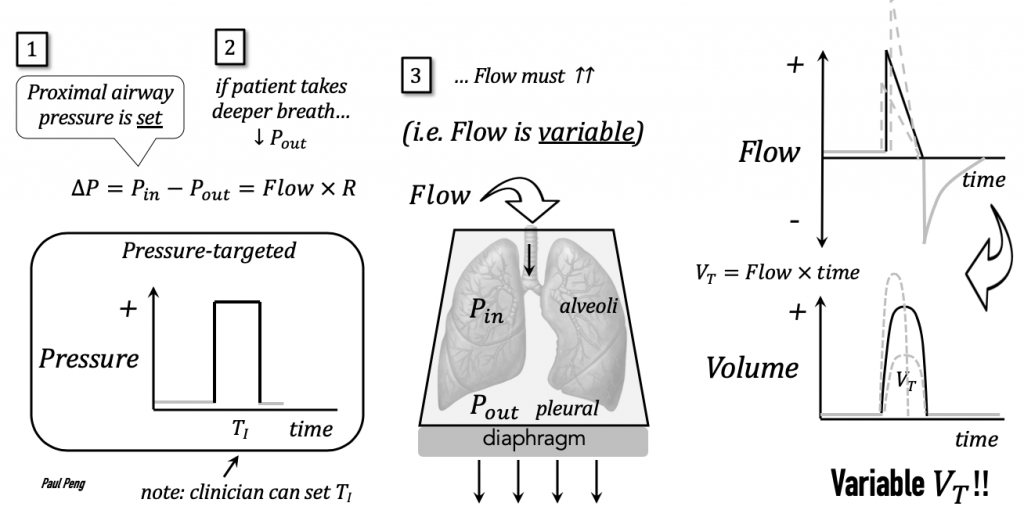
- A pressure-target will allow FLOW (Volume) to vary.
- If patients are generating significant efforts at inspiration (“air hunger”), then this mode may be more comfortable because it gives the patient what he/she “wants”.
- Be careful with variable volumes! Must ensure that patient is receiving lung-protective ventilation (or enough volume).
Another confusing topic is the I:E ratio.
In A/C-V mode, it is determined indirectly by the flow rate and tidal volume that is set.
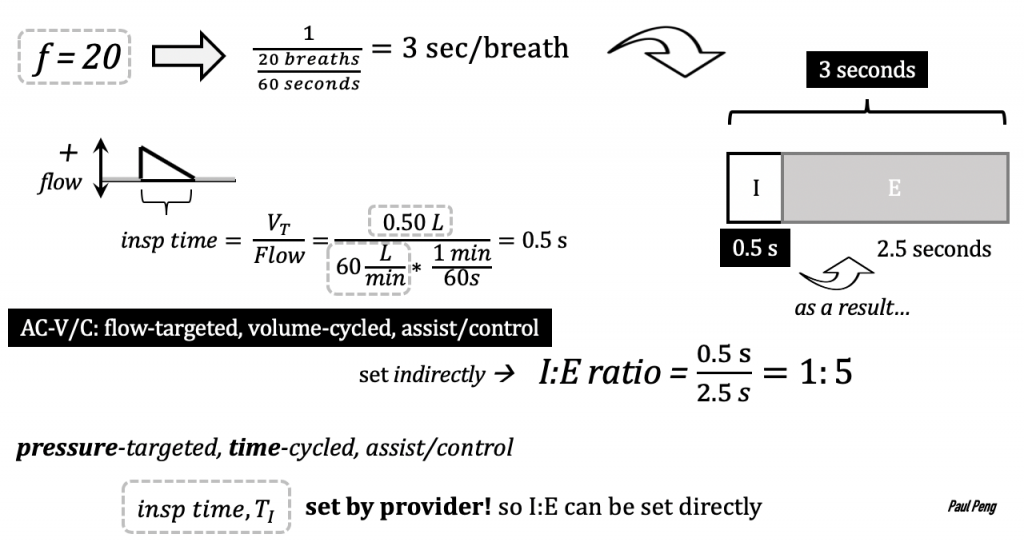
What happens if you increase the flow rate? TI shortens and expiratory time lengthens. This is sometimes desirable if intrinsic PEEP (stacked breaths) is an issue (e.g. COPD / asthma).
Putting it all together…
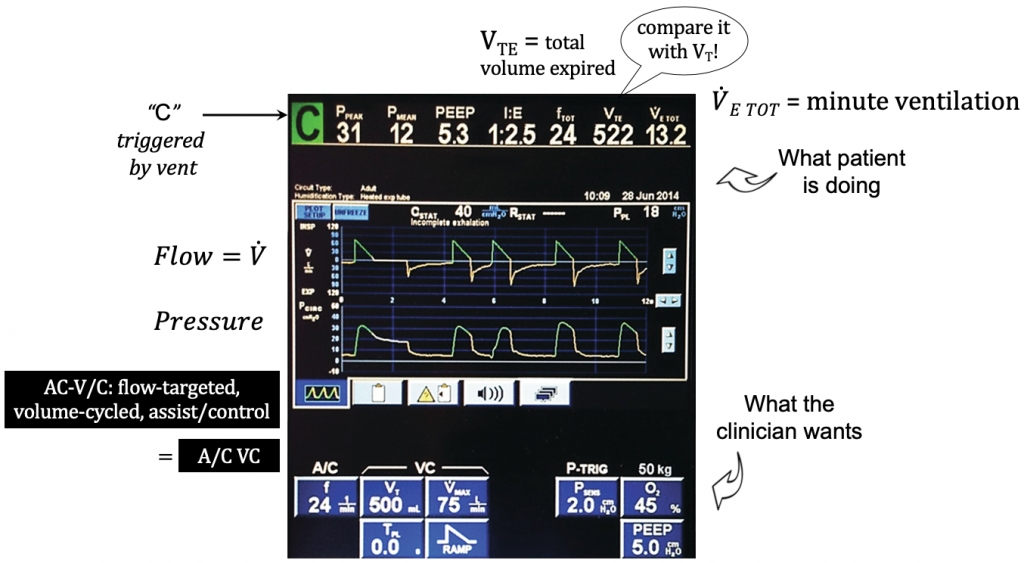
Extra parameters that are less-often used (with the exception of VMAX):
- VMAX: peak flow rate,
- increase for patient comfort (e.g. match high inspiratory effort)
- increase will allow longer expiratory time
- try increasing or decreasing if patient is double-triggering
- TPL: plateau time, extends inspiratory pause (see the next post: ventilator alarm)
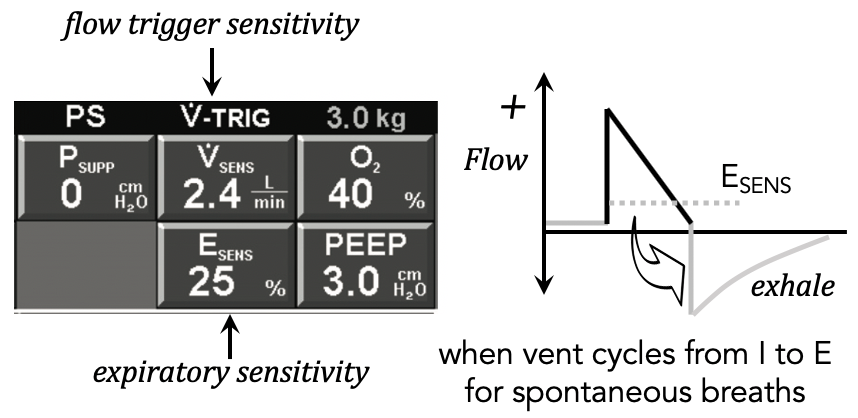
- ESENS: percent of peak flow rate, when to cycle I to E
- VSENS: how easy it is for patient to trigger flow
References
Wilcox S.R., Aydin A., Marcolini E.G. Mechanical Ventilation in Emergency Medicine.
Martin J. Tobin. Principles and Practice of Mechanical Ventilation, 3e
J. M. Cairo. Pilbeam’s Mechanical Ventilation: Physiological and Clinical
Michael G. Levitzky. Pulmonary Physiology, 9e
Hooman Poor. Critical Care Lectures.
Jesse Hall. Principles of Critical Care, 4e
Scott D. Weingart. Managing Initial Mechanical Ventilation in the Emergency Department.
