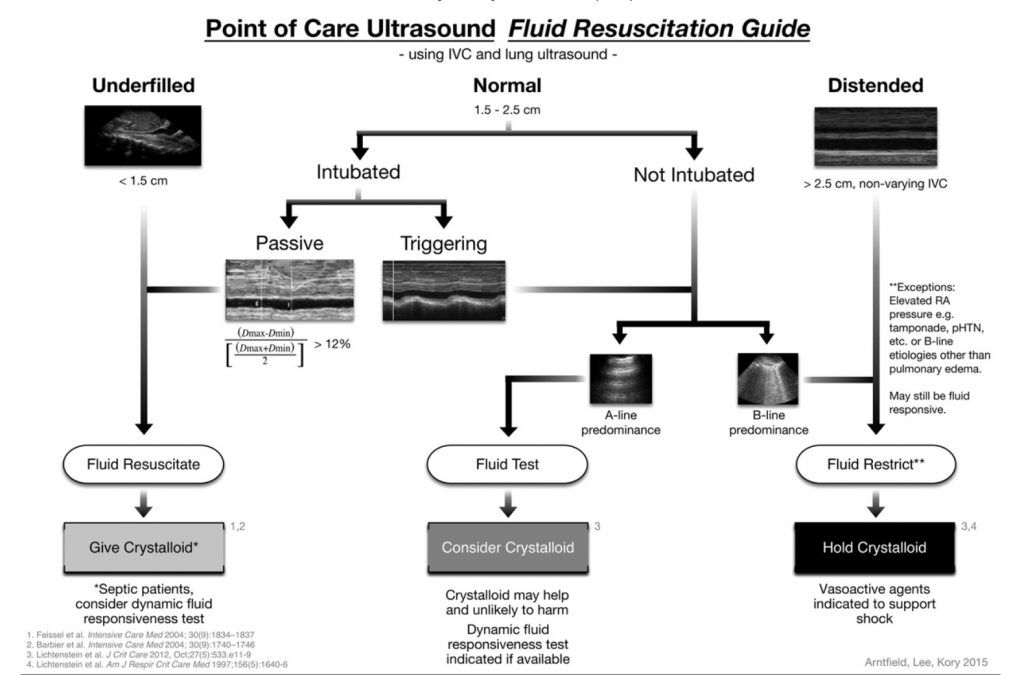
Tanking up the volume-depleted hypotensive patient requires a fine balance between under-resuscitation and the pulmonary edema of overdoing it. “Dynamic” measures of fluid responsiveness are technically complex and likely inaccessible to most ED physicians, so consequently much research and discussion has offered ultrasound techniques of varying degrees of complexity for assessing volume status. Here’s a recently proposed algorithm (Journal of Critical Care, citation below) for you to utilize on your next non-ventilated patient that incorporates the growing body of literature on the topic
And here’s the basic principal behind it: Correlating IVC collapsibility directly to fluid responsiveness has only been proven to work in mechanically-ventilated patients, so the above algorithm focuses on the maximal diameter of the IVC at the high and low end of the spectrum.
<1.5 cm diameter= good data to suggest that these patients will respond to fluid
>2.5 cm= good data to suggest that these patients won’t respond to fluid.
If a non-intubated patient has an IVC diameter in the middle range (1.5-2.5 cm) , they deserve a trial of additional fluid (or assessment with a simple passive straight leg test), unless their lung ultrasound reveals B-lines, an early pre-radiographic and pre-clinical B-lines finding of a positive fluid balance.
Thanks to local ultrasound guru Phil Andrus for the guidance.
Lee C, Kory P, Arntfield R. “Development of a fluid resuscitation protocol using inferior vena cava and lung ultrasound.” Journal of Critical Care. 31 (2016) 96–00