Syphilis
Written by Erena Weathers
What is syphilis?
It is an infection caused by the bacterium Treponema pallidum, a spirochete, with an internal flagella. You may know it as the GREAT IMITATOR but it is also known as the GREAT POX (and that is why smallpox is called smallpox, because syphilis took the title of the great pox). It is spread through sexual contact (wrap it up) and vertical transmission (mama to bebe).
How do we test for it?
I recommend the “reverse syphilis test algorithm” in which you do a treponemal test followed by a non-treponemal test (RPR/VDRL).This starts with an assay to measure specific IgM and IgG antibodies to Treponema pallidum. The advantages are that T. pallidum antibodies (TPA) are 1) specific to syphilis, 2) are more sensitive than VDRL or RPR for detecting both primary and late syphilis, 3) can be tested using automated instruments, and 4) can provide a more rapid time to result.
Neurosyphilis: this is the exception where it is still recommended to obtain that CSF (get ready to pop some champagne), and test CSF-VDRL which is the gold standard. If the CSF-VDRL is non-reactive, and neurosyphilis is suspected, a CSF FTA-ABS can be ordered. Although it is less specific than a CSF-VDRL, the CSF FTA-ABS test is quite sensitive, and neurosyphilis is highly unlikely with a negative CSF FTA-ABS test.
Why test for it?
IT’S EVERYWHERE AND EASILY TREATED. Like it is skyrocketing after a decline in the early 2000s. I recommend screening all your sexually active patients with GU complaints, as well as those who come in just for GC screening.
How to treat?
- Primary, Secondary, or Early Latent (<1 year): Benzathine penicillin G 2.4 million units IM in a single dose
- Late Latent (>1 year), Latent Syphilis of Unknown Duration, or Tertiary Syphilis with Normal CSF Examination: Benzathine penicillin G 7.2 million units total, administered as 3 doses of 2.4 million units M each at 1-week intervals
- Pregnant women: Pregnant women should be treated with the penicillin regimen appropriate for their stage of infection. Additional doses of penicillin in pregnant women with early syphilis may be indicated if evidence of fetal syphilis on ultrasound.
- Neurosyphilis, Ocular Syphilis: Aqueous crystalline penicillin G 18–24 million units per day, administered as 3–4 million units IV every 4 hours or continuous infusion for 10–14 days.
- Congenital syphilis: there is a one day vs 10 day course for infants, and I would defer to peds ID on this one.
History time
From the 1920s until the 1950s, prior to the introduction of penicillin, malaria-induced fevers were used as a treatment for neurosyphilis. This was called pyrotherapy, in which patients with neurosyphilis were infected with P. vivax (malaria), and then anti-malarial drugs were used to control the P. vivax infection while maintaining the fever to kill the spirochetes in the brain. Dr. Julius Wagner-Jaureggn won the Nobel Prize for Medicine in 1927 for his elaboration of the procedure in treating neurosyphilis.
Sad History Time
Lest we forget, the Tuskegee Trial was an ethically abusive study conducted between 1932 and 1972 by the United States Public Health Service (PHS) and the Centers for Disease Control and Prevention (CDC) on a group of nearly 400 African Americans with syphilis. The purpose of the study was to observe the effects of the disease when untreated, though by the end of the study it was entirely treatable. The men were not informed of the nature of the experiment, and more than 100 died as a result. None of the infected men were treated with penicillin despite the fact that, by 1947, the antibiotic was widely available and had become the standard treatment for syphilis. On May 16, 1997, President Bill Clinton formally apologized on behalf of the United States to victims of the study, calling it shameful and racist.
Interesting Reactions
Be careful, and be on the lookout for a Jarisch-Herxheimer reaction. The Jarisch-Herxheimer reaction generally consists of fever 2 to 12 hours after initiation of therapy for active syphilis and is not a reaction to the antibiotic, and you should counsel the patient that this can be a normal reaction to therapy and does not mean they have a penicillin allergy. However, cardiovascular collapse, seizures, and death also have been reported. The Jarisch-Herxheimer reaction is thought to be produced by the release of endotoxin-like compounds during penicillin-mediated lysis of T. pallidum. Dr. Megha George had a case of this in fast track, so you will probably see this!
What are these stages?
Primary: One or more chancres (usually firm, round, small, & painless but can be atypical, subtle lesions) are thought to appear at the site of exposure (mainly genital area) ~3 weeks after infection (range 10–90 days). Chancres can heal on their own in a few days to weeks, even without treatment. The patient is highly infectious, and in utero transmission is likely in pregnant women.
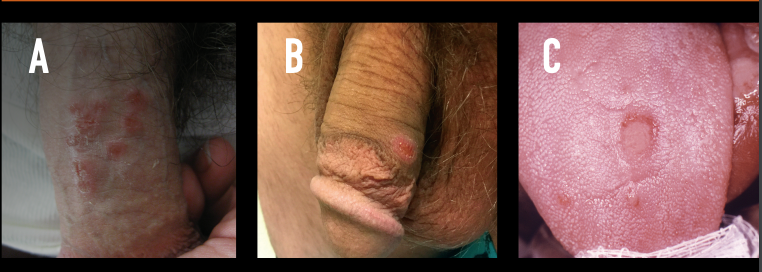
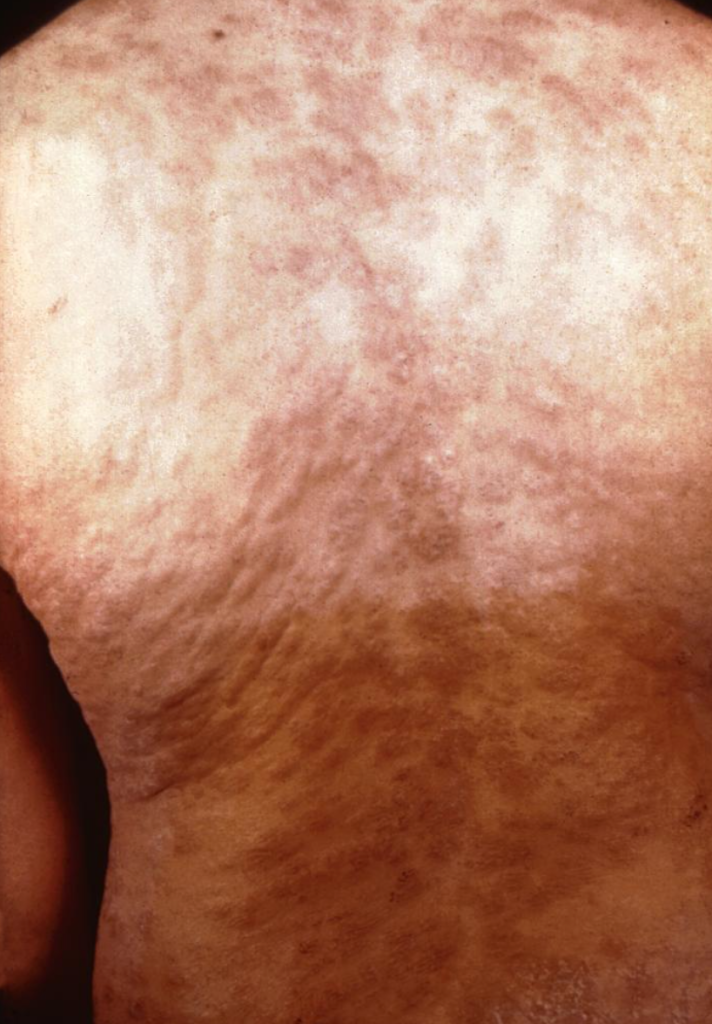
Secondary: Mucocutaneous lesions (most commonly rashes) can occur as chancre(s) fade ~6 weeks after infection (range 3 wks–6 mos). Rashes may first appear on the palms of hands or the soles of feet but typically appear on the trunk and other areas of the body. Lesions such as condyloma lata, a moist, wart-like lesion found in the genital area, and mucous patches on the tongue occur in ~25% of patients. Other common findings: lymphadenopathy & constitutional symptoms. Less common: patchy alopecia (~10% of patients) & neurologic symptoms (1–2% of patients). Symptoms clear within 2–6 wks but may take up to 3 mos, even without treatment. The patient is highly infectious, especially if direct contact with a moist lesion. In utero transmission is likely in pregnant women.


Latent Stages:
Early latent: The patient has reactive nontreponemal and treponemal tests within 1 year of onset of infection, but no symptoms. The patient is potentially infectious, as signs of primary & secondary syphilis can reoccur and go unnoticed.
Late Latent or Latent of Unknown Duration: The patient has reactive nontreponemal and treponemal tests ≥1 year after the onset of infection, or the onset of infection cannot be determined but the patient has no symptoms. The patient is not infectious in the late latent stage but may be infectious in the latent stage of unknown duration if the onset of infection was within the past year.
Tertiary: Manifestations in skin and bones (gummas) and the cardiovascular system. The patient is not infectious.



Neurosyphilis: Neurosyphilis is a site of infection and can occur at any stage of syphilis. The nervous system is infected within hours after infection but it can take weeks or years before symptoms present, if at all. All patients with syphilis and neurologic, ophthalmologic, or audiologic symptoms warrant a careful neurological exam and a CSF evaluation via a lumbar puncture (LP). All patients at high risk for syphilis presenting with neurologic symptoms should be tested for syphilis and HIV.
Early neurosyphilis usually presents a few weeks or a few years after the onset of infection and can occur at the primary and secondary stages. It typically manifests as meningitis that can affect cranial nerves (especially VI, VII, and VIII), and as meningovascular syphilis which may present with stroke-like symptoms.
Late neurosyphilis typically presents 10–30 years after the onset of infection at the late latent stage. Manifestations include general paresis (chronic meningoencephalitis leading to dementia, muscle weakness, and paralysis) or tabes dorsalis (demyelination of the posterior columns of the spinal cord).
MOAR HISTORY: You have probably heard that old-timey dictators and kings were afflicted with neurosyphilis. Here’s looking at you King Henry VIII, Tsar Ivan IV Vasilievici (Ivan the Terrible), and others. But did you know about Al Capone too?
Ocular Syphilis: Ocular syphilis can occur at any stage of syphilis. Visual complaints consist of vision loss, blurry vision, eye pain, eye redness, etc. Patients at high risk for STIs who present with ocular signs or symptoms should be tested for syphilis and HIV. Patients with syphilis & ocular symptoms should receive a careful neurological exam, an ophthalmologic assessment, and CSF evaluation via lumbar puncture. Treatment should not be delayed while awaiting the results of tests as severe outcomes, including permanent blindness, have been reported.
Congenital Syphilis: Approximately 60 to 90 percent of live-born neonates with congenital syphilis are asymptomatic at birth. The presence of signs at birth depends upon the timing of intrauterine infection and treatment. Among symptomatic infants, the most common findings include hepatomegaly, jaundice, nasal discharge (“snuffles”), rash, generalized lymphadenopathy, skeletal abnormalities.
References
“Pyrotherapy.” Wikipedia, Wikimedia Foundation. 18 Oct 2021. https://en.wikipedia.org/wiki/Pyrotherapy
“Tuskegee Syphilis Study.” Wikipedia, Wikimedia Foundation. 19 Nov 2021. https://en.wikipedia.org/wiki/Tuskegee_Syphilis_Study
Tampa M, Sarbu I, Matei C, Benea V, and Georgescu SR. “Brief history of syphilis.” J Med Life. 2014. 7(1):4-10.
Center for Disease Control and Prevention. “Syphilis: Pocket Guide for Providers.” US Department of Health and Human Resources. Oct 2017. https://www.cdc.gov/std/syphilis/Syphilis-Pocket-Guide-FINAL-508.pdf
Dobson SR, Kaplan SL, and Weisman LE. “Congenital syphilis: Clinical features and diagnosis.” UpToDate. 26 Mar 2021. https://www.uptodate.com/contents/congenital-syphilis-clinical-features-and-diagnosis
