Will Artificial Intelligence take over my job? Not likely in the immediate future!
Can it help me right now to make more evidence based decisions in my daily practice? Possibly!
Now that artificial intelligence (AI) tools have become ubiquitous in our society, you may be asking yourself how you can use these tools to make your life easier. In this short pearl, we will explore one tool, Open Evidence, and how you may use it to help answer some questions on your next shift.
Open Evidence is an AI powered web-based platform that, much like ChatGPT, has the ability to aggregate and synthesize literature and present information in a way that helps clinicians make evidence-based decisions.
To be very clear… Open Evidence is an experimental technology that CANNOT fully substitute your clinical judgement and assessment of current guidelines/literature when making clinical decisions.
According to the Mount Sinai Levy Library:
“OpenEvidence is one source, and as an experimental learning tool, should not be the only source of information you consult. It’s crucial to check what the original references say and document the AI-generated information… All AI systems may make errors, and without knowing which sources it is consulting, you should continue to compare outputs with trusted sources to ensure you have obtained the highest level of evidence for your clinical questions.”
Now that we have that out of the way….
Let’s dive into an example of how you can use this tool on shift..
You are considering a patient’s risk factors for PE. She mentions that she uses a NuvaRing. You remember that estrogen-containing OCPs increase PE risk, but you are curious if there might be a difference in risk based on the route of hormone administration.
You are also busy on shift and don’t have enough time to sift through pubmed articles or practice guidelines….
So, you log into Open Evidence and start thinking of a prompt.
You come up with a PICO question (Population, Intervention, Comparison, Outcome)
In women of reproductive age, does the use of a NuvaRing, compared to oral estrogen contraceptive use decrease the risk of pulmonary embolism?
You plug it into Open Evidence… and here is your response..
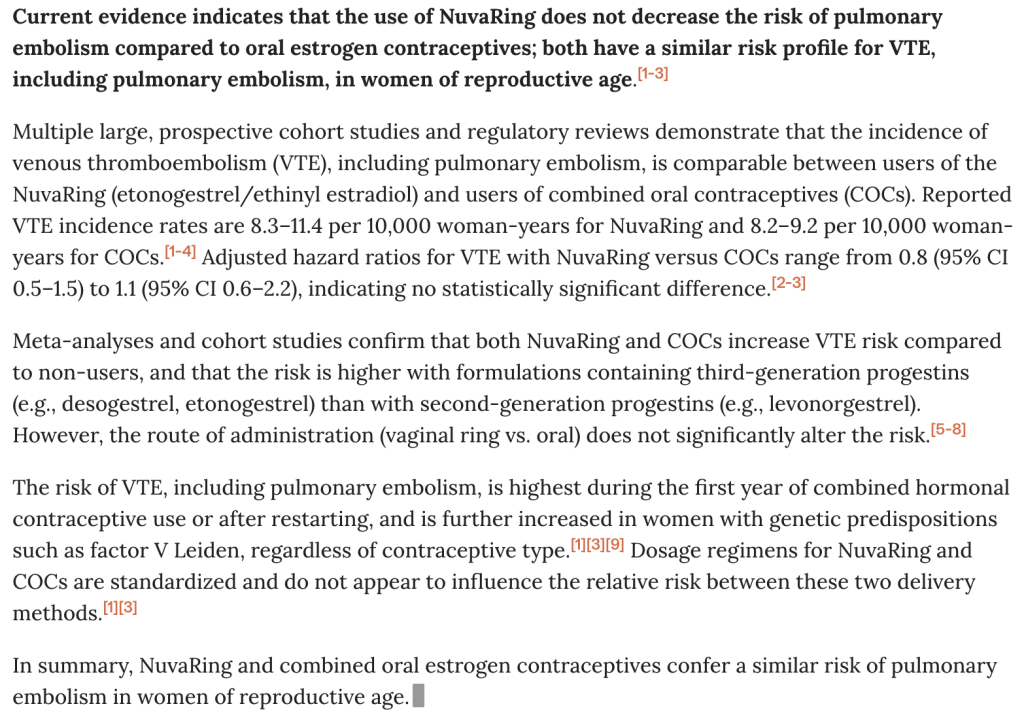
So there we have it… Your patient who uses a NuvaRing has similar PE risk to those taking estrogen containing oral contraceptives.
Before you move on, you should confirm the information generated in the output by referencing the sources and making sure that the articles are legitimate and reflect the generated content!
How do I make an account?
Simple! Register online here and make sure to have your NPI number (search for yours here)
Additional Reading: Prompt Engineering for Medical Professionals
