Headaches are the most common complication of doing a lumbar puncture (LP). Let’s dive into what causes them, how to prevent them, and what to do when patients come back suffering from a post-LP headache.
Some major theories on why post-LP headaches develop:
Cause of the post-LP headaches is still highly debated!
Theories:
- Continued loss (leakage) of CSF through the puncture site > pressure changes
- Loss of CSF “cushion” on the brain > traction on meninges, cranial nerves, bridging veins, & cervical structures which are sensitive to pain
o Cool correlations: Traction on: trigeminal nerve > frontal headache; abducens nerve > visual sxs; vagus nerve> nausea, cervical nerves > pain in neck + shoulders - Losing CSF at higher rate than producing it > body responds to try to maintain a constant cerebral volume by intracranial venous dilation > increased volume in closed space (skull)> neurohumoral response identified as pain
Timeline:
- Symptoms can occur immediately after LP to several days or even weeks after
- 90% occur within first 48 hours after LP
- Cases have been reported at two weeks post-LP
- In rare cases even up to several months! Yikes!
Demographics:
- Most commonly occurs in ages 18-30, decreased incidence after age 60 (unclear reasons: perhaps small amount of cortical atrophy > more room, less pressure?)
- More common in female sex, low BMI
- Migraine history does not increase risk
- Obesity seems to be protective
Headache characteristics:
- Headache often dull, bilateral, vague discomfort exacerbated by posture changes (worse with sitting up or standing, improved with supine position)
- Associated symptoms can include: nausea, vomiting, tinnitus, neck stiffness, photophobia
Prevention:
- Higher risk of developing post-LP headache if larger diameter needle or cutting needle used & higher incidence with repeated LP attempts (repeat dura punctures)
- So use a small-diameter, blunt needle to help prevent post-LP headache
- Bevel should be parallel to the longitudinal dural fibers
- Replace stylet prior to removing the needle
- Early ambulation has NOT been shown to increase incidence!
- Incidence also does NOT seem to be related to: opening pressure, volume of CSF removed, or bed rest after the LP
Management:
Initial management: NSAIDs, can also try IV fluids
Headache refractory to treatment: caffeine may be effective
- single dose of 300 mg oral caffeine
- for more severe headache: 500 mg IV caffeine sodium benzoate
- Some data with success rate w/ caffeine as high as 70%, however efficacy controversial
- Theory behind effectiveness of caffeine: caffeine acts as vasoconstrictor; theory above is vasodilation = part of etiology of post LP headache
- People are trying some interesting things! that show possible effectiveness, but aren’t (yet) mainstream: gabapentin, hydrocortisone, theophylline, triptans, cosyntropin (an ACTH anaong), as well as occipital nerve block…cool stuff
The epidural blood patch: what is this mystical, strange & unusual treatment option?!
- Has been in use for over 50 years
- A little history: Gomley first described this technique for managing post-LP HA in 1960, became widely used a decade later
- Continues to be the “gold standard” treatment for post-LP headache
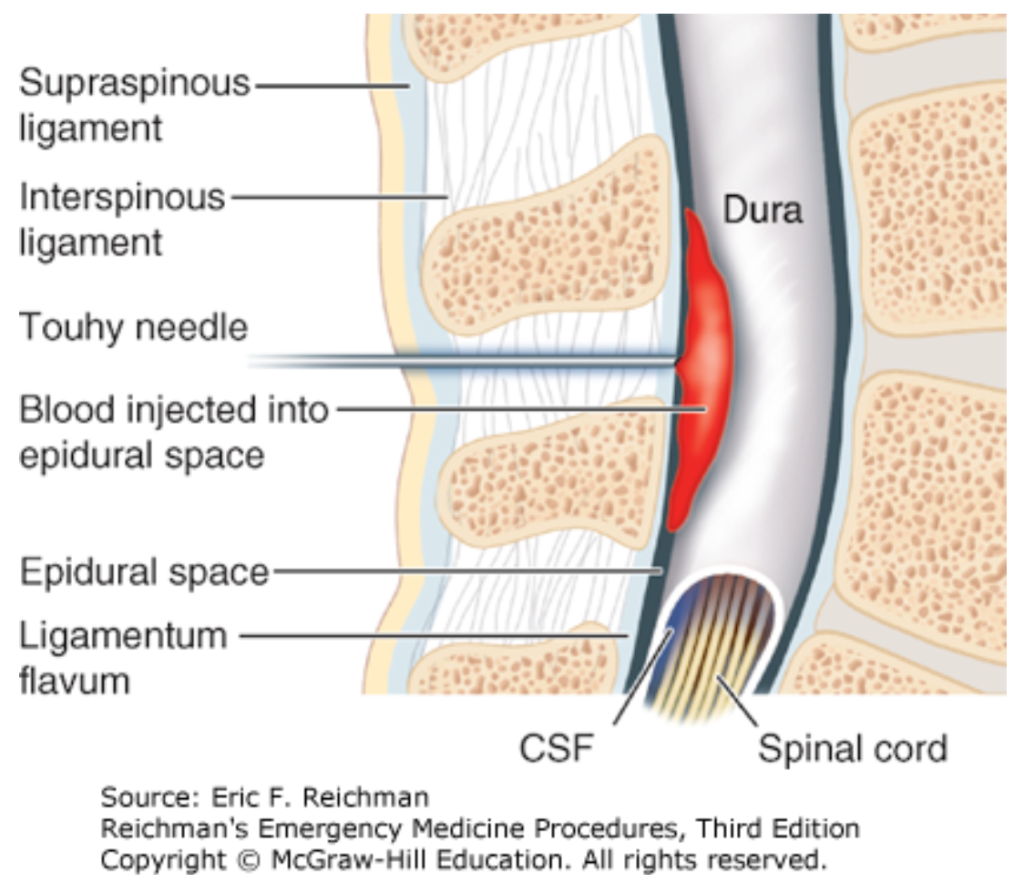
- If all else above fails: consider epidural blood patch: blood from patient (autologous blood) injected into the epidural space, clots, forms a plug to stop LP leak! Also thought to increase ICP by mass effect
- This is last-line as it is invasive
- Typically performed by anesthesiologist
- Involves injecting 15-20 cc patient’s blood into epidural space at the level of the previous LP
- Tamponades further CSF leakage, enables healing of the dural opening
- Success rate about 85% after one injection, 98% if 2nd patch required
- Should not be performed sooner than 24 hours post-LP, though is more effective the earlier in post-LP course that it is performed
- Transient complications: back pain, paresthesias, radiculopathies, weakness
- Rare complication – spinal subdural hematoma
- Absolute contraindications: active infection at site, sepsis, bacteremia, meningitis
- Caution in patients w/ cancer or immunodeficiency
Further reading on how the epidural patch is actually performed:
https://accessemergencymedicine-mhmedical- com.eresources.mssm.edu/content.aspx?bookid=2498§ionid=201296783#1159804497
Reichman’s Emergency Medicine Procedures Chapter 143: Blood Patching for Postdural Puncture (Lumbar Puncture) Headache