Intro
Case Introduction: You are the overnight Peds EM resident and at 3 o’clock in the morning you get a notification (~5 minutes away) that a 4 month old boy with a hx of Tetralogy of Fallot who is awaiting elective repair is coming in appearing severely cyanotic, crying loudly, and hypoxic to ~40%. After hearing the notification, the heart rate on your apple watch immediately reads ~150. You brace yourself for when this 4 month old enters into your bay. What are you going to do?
Tl;Dr Pearls – <5 minutes
This is the order of operations “PEM”DAS version of how you would treat and escalate care for this patient. Pun is intended
- Within <5-10 minutes
- Place patient on monitor and obtain initial vital signs
- Obtain IV Access
- Place patient on Nasal Cannula or Non-Rebreather oxygen mask
- Have patient “squat” or manually place knees to chest position
- Normal Saline Bolus
- Within <30 minutes, consider these options for escalation of care:
- Morphine IV/IM
- Phenylephrine IV
- Esmolol or Propranolol IV push followed by gtt
- Bicarbonate IV push or gtt for severe acidosis while preparing for an intubation
- Consider Ketamine while preparing for an intubation
Read more below for some pathophysiology of why you are approaching a Hypercyanotic “Tet” Spell with this approach
Extended Pearls – >5 minutes
Tetralogy of Fallot is a congenital heart defect impairing normal blood flow defined by these 4 defects:
- Pulmonary Stenosis – Narrowing of the pulmonary valve causing an obstruction of blood flow from right ventricle to pulmonary circuit
- Right Ventricular Hypertrophy – Thickening of RV wall because of constant high pressure RV is exerting to push blood flow
- Ventricular Septal Defect (VSD) – A hole between the right and left ventricles
- Overriding Aorta – The aortic valve is enlarged and appears to open from both the right and left ventricle instead of just normally the left ventricle
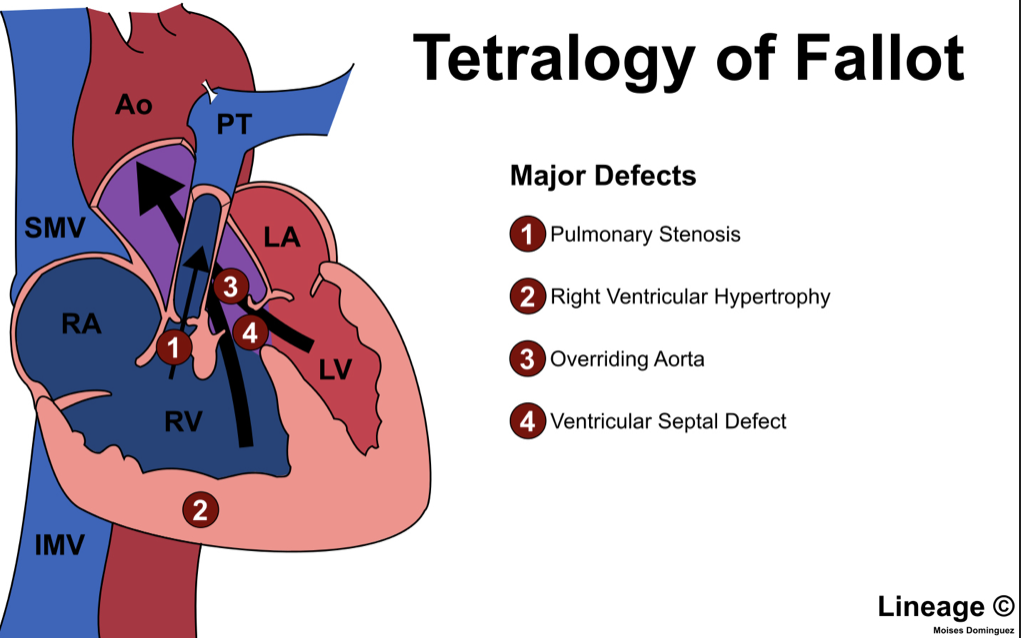
Oxygen poor (blue) blood in the right ventricle is obstructed by pulmonary stenosis allowing for an abnormal flow through the VSD into the left ventricle and ultimately into the overriding aorta. This mixes with oxygen rich (red) blood to enter systemic circulation. This “shunting” of blood results in reduced arterial oxygen saturation and a cyanotic baby. The more pulmonary stenosis and narrowing of the RV ventricular tract = more cyanosis.
What causes a TF Spell/Hypercyanotic Spell? Various triggers (i.e child crying, being more active, etc..) can cause a sympathetic stimulation/catecholamine release that 1.) Causes more contraction of right ventricular outflow 2.) Increases heart rate and cardiac output causing more deoxygenated blood to enter into the systemic circulation. As a result, decreased arterial oxygen content triggers acidosis and hypercapnia. This in term creates a vicious cycle of cardio-respiratory deterioration = Hypercyanotic Spell or “Tet” Spell.
Management
The principles of management regarding this patient who is cyanotic and hypoxic to ~40% will be based on 1.) Establishing a calm environment for the patient (i.e decrease catecholamine production) 2.) IV Fluids for volume expansion 3.) Increasing SVR 4.) Reversing the tachycardia
- Establishing a calm environment: This is crucial because you want the patient to be more relaxed and not in a crying state
- Having a child life specialist play a role here is crucial. You can also have the patient sit in a family’s members lap for them to feel more comfortable
- Application of a Non-Rebreather mask. Also helps to reduce pulmonary vascular resistance
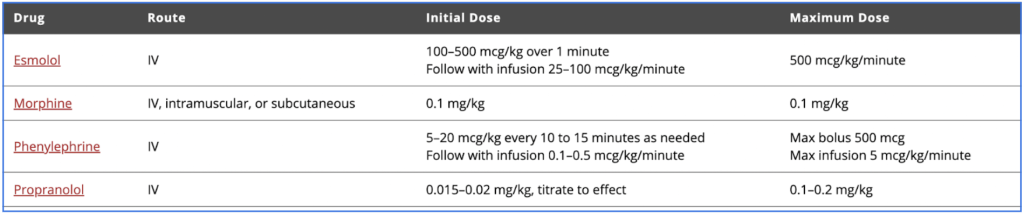
- Morphine (.025-.05 mg/kg IV/IM)
- IV Fluids: This helps to both improve preload as well as overall end diastolic volume of the right ventricle
- NS 10ml/kg bolus
- Increasing SVR: By improving the systemic vascular resistance you are increasing the pressure in the Left Ventricle thus reversing the “shunt” allowing deoxygenated blood to enter into the pulmonary circuit and become more oxygenated
- By having an infant “squat” or manually pushing their knees against their chest you are manually increasing the SVR
- Phenylephrine (5-20 mcg/kg q 10 minutes IV) is a pure alpha-agonist leading to arterial vasoconstriction and thus increased SVR
- Ketamine can also be used as an adjunct for both increasing SVR and having a sedative effect
- Reversing Tachycardia: By lowering the heart rate of the patient, you are allowing for improved cardiac filling and preload. Also will decrease infundibular spasm (region below the pulmonary valve)
- Esmolol (100-500 mcg/kg over 1 minute IV)
- Propranolol (.015-.02 mg/kg IV)
Disposition: An unstable patient such as this that was resuscitated should be admitted to the PICU. In the long-term, these patients need surgical corrective repair of their ventricular septal defect as well as enlargement of their pulmonary valve within the first 1st year.
Further Resources
https://www.cincinnatichildrens.org/health/t/tof
