As the stellar EM provider that you are, you’ve probably gotten pretty great at independently reading CTs, XRs, and even formal ultrasounds at this point.
But what about the mysterious MRI? You know your consults need them, the radiologist will eventually read them, but it’s something that we don’t do ourselves quite often enough, usually putting in the order before we send them to observation, right after a stroke code, or as we press the “admit” button after the radiology read. Here, we go over the basics.
How do they work?
In brief, MRI, or Magnetic Resonance Imaging, uses a giant magnet to line up the positively charged hydrogen ions, largely located in your water-dense soft tissue (which is why MRI is so great at visualizing these areas of your body). For tissue/material with different compositions, these hydrogen ions will react differently to said magnetic field, requiring additional energy input to synchronize, which is provided in the form of radiofrequency (RF) waves. This energy is then discharged, the varying strengths of which are then measured by the machine and reconstructed into a 3D image via computer software, a process called Nuclear Magnetic Resonance (NMR).
Terminology
MRI images are greyscale, with whiter structures referred to as “hyperintense” and blacker structures “hypointense”.
Benefits
Often used for a more sensitive 3D look at soft tissue structures (i.e. your brain, spinal cord, ligamentous tears, tendon ruptures). Can also “suppress” certain signals for a more targeted and customizable search.
Cons
Contraindicated if any metal in the body, permanent piercings, metal-based tattoo ink, metallic medical devices. Takes a long time, anywhere from 15mins to more than an hour. Expensive compared to CT. Children and people with significant claustrophobia may require a sedation regimen.
Sequences: Probably the most confusing part of reading MRIs. Which one do I pick? What am I looking at? Why is that part lighting up? I’ll cover 4 main ones.
- T1: Highlights FAT, like the fatty myelin-insulated axons of white matter. The most “anatomical”, meaning it appears most similar to the tissue’s actual appearance. Usually used as a comparison study, most commonly with T2.
- Gadolinium-enhanced: contrast studies are in T1, enhances inflammation, vasculature, malignancies (just like in CTs)
- Fat-suppression: can be used to diminish glare from bright fatty tissue to better bring out contrast-enhanced regions in gadolinium studies
- T2: Highlights WATER (i.e. CSF, but also edema, infection, post-infarct/ischemic changes, aka. bad things). Reverse of T1, fats appear dark (except in bone marrow and adipose tissue) and water is lit up.
- STIR (Short Tau Inversion Recovery): aka. fat-suppression in T2 to better assess bone marrow pathology and possible edema in fatty areas (e.g. spinal lesions)
- FLAIR (Fluid Attenuated Inversion Recovery): similar to T2 (water bright, fat dark), BUT darkens the otherwise bright CSF, very useful in evaluating pathology in CNS (especially periventricular, sulci, and gyri, aka. Areas adjacent to what would have been otherwise glaring CSF)
- DWI (Diffusion Weighted Imaging): detects extracellular random water molecule proton movements, which is severely restricted in acutely ischemic tissue, resulting in a bright signal (diminishes after weeks), extremely sensitive in detecting acute strokes (think negative CTs, but high suspicion for stroke)
Examples:
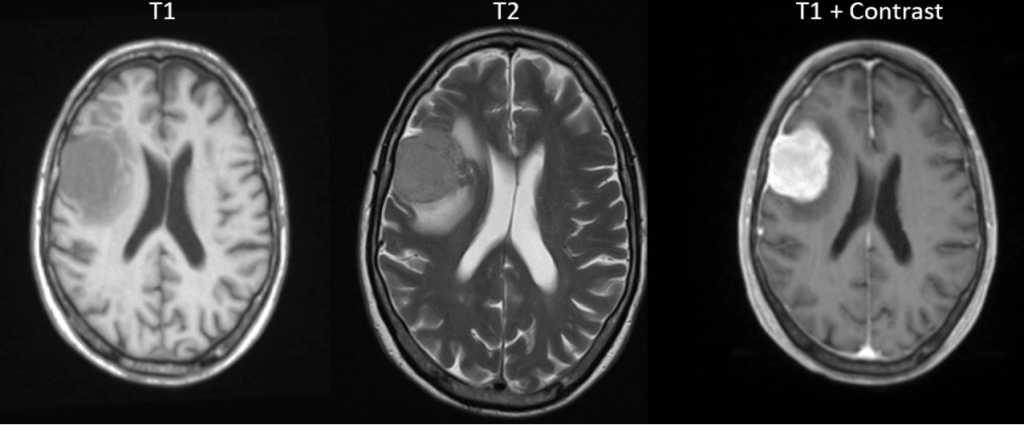
Meningioma: hypointense T1 given lack of fatty tissue, hypointense T2 but with hyperintense surrounding edema, gadolinium-enhanced with continuation into dura mater
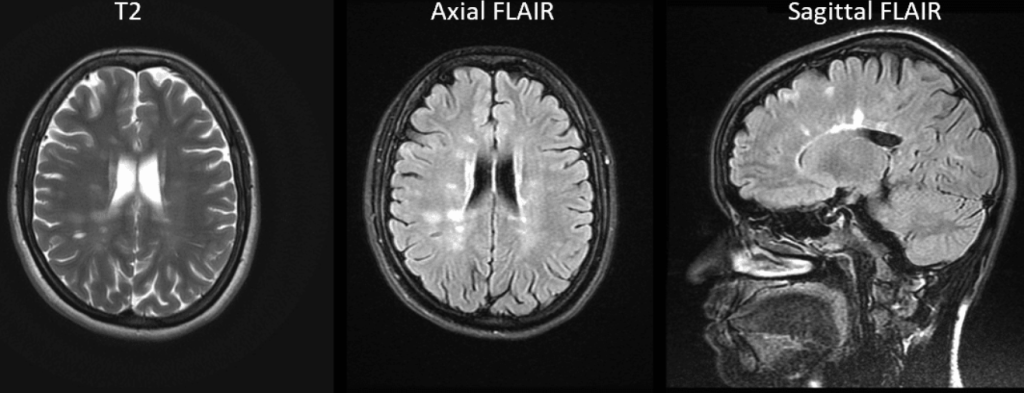
Multiple Sclerosis: scattered patchy areas of periventricular hyperintensities, more apparent on FLAIR sequence in absence of CSF enhancement
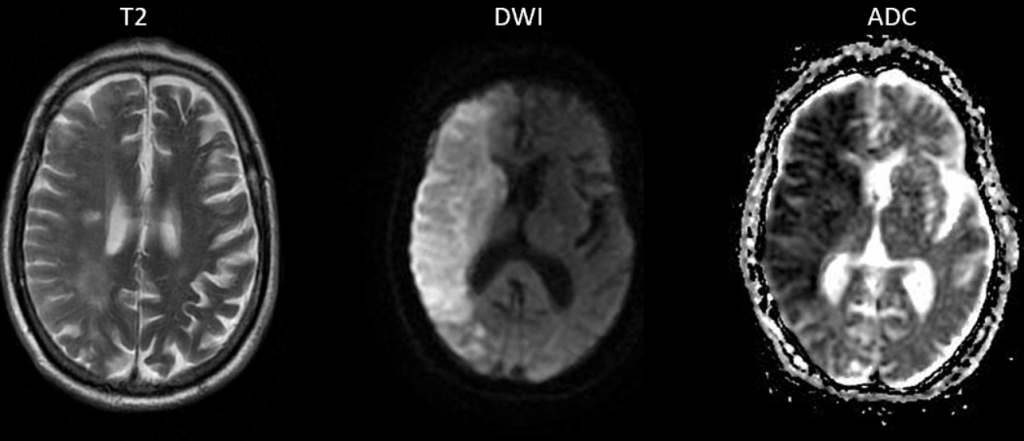
R-sided ischemic stroke: visible DWI enhancement to the acutely ischemic region of R hemisphere, always correlated with confirmatory ADC (Apparent Diffusion Coefficient), but don’t worry about that.
TL;DR:
T1: FATS, study for comparison and when using contrast
T2: WATER, most versatile for various pathology
FLAIR: T2 but especially for CNS + CNS adjacent spaces
DWI: Acute stroke, bright = ischemia
I acknowledge this merely grazes the surface of reading MRIs, but I hope it gives you something to work off of and gently pushes you on your journey towards interpreting your own MRIs before the overnight neuroradiologist does!
