Summary
Summary
- The Lisfranc joint is made of the first four metatarsals, cuneiforms and cuboid and associated ligaments
- A Lisfranc injury is any disruption of the joint
- The mechanism of injury (axial load on plantarflexed foot, rotational force, crush injury) should increase suspicion for this injury
- Familiarize yourself with the normal foot x-ray as findings for a Lisfranc injury can be subtle
- Management depends on the severity of injury and should involve a discussion with your orthopedic surgery colleagues
- Stable nondisplaced injuries, including ligamentous injuries, can be discharged with a short leg cast, NWB status, crutches and outpatient orthopedic surgery follow up
Anatomy of the Lisfranc Joint
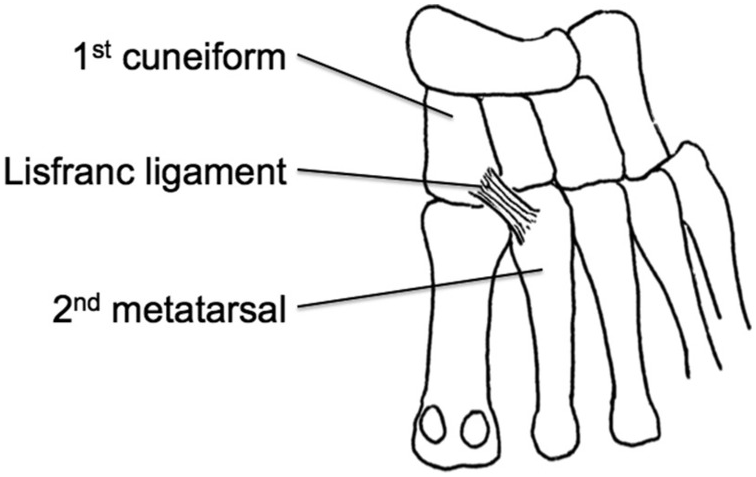
The Lisfranc joint consists of the articulation of the first three metatarsal bases with their respective cuneiforms and the 4th/5th metatarsal bases with the cuboid, along with associated ligaments. The lisfranc ligament, which joins the medial cuneiform (1st cuneiform) and the base of the 2nd metatarsal, provides primary structural support to the joint.
The Lisfranc Injury
The lisfranc injury is any disruption of the joint and is a spectrum including ligamentous injury, dislocations and fractures.
Mechanism of Injury
The key to diagnosis is in the history. Lisfranc injuries can occur with axial loads of the plantarflexed foot (e.g. stepping into a pothole or high speed MVC with foot on pedal), rotational forces on the foot (e.g. equestrian falling off a horse with foot caught in stirrup) or crush injuries. High energy mechanisms, such as MVCs or falls, are more likely to cause fracture-dislocations. Whereas low energy mechanisms are associated with ligamentous injuries.
Symptoms and exam
Depending on the severity of injury, patients may have:
- pain or swelling, particularly over the lisfranc ligament
- inability to bear weight
- absent dorsalis pedis pulse (if there is vascular injury).
- pain with passive plantar and dorsiflexion of the foot (Piano Key test)
- pain with passive abduction and pronation of the forefoot with the hindfoot held in the other hand
- Plantar ecchymosis
Imaging
Foot x-rays should include AP, lateral and oblique views. Ideally, include weight-bearing films when there is high suspicion for a lisfranc injury based on mechanism and exam. Obtain CT imaging if the patient cannot tolerate a weight bearing film or there is high clinical suspicion for injury. Familiarize yourself with the normal foot x-ray so you can learn to detect the subtle findings associated with a Lisfranc injury.



Image source: radiopaedia.org
What to look for on imaging:
- AP: alignment of the first and second metatarsals and cuneiforms, distance between the bases of the first and second metatarsals should be less than 2 mm
- Oblique: alignment of the third and fourth metatarsals with the cuboid and lateral cuneiform
- Lateral: dislocation in the plantar or dorsal directions
- Fleck sign is an avulsion fracture of the second metatarsal or medial cuneiform and associated with a Lisfranc injury
Here is a gallery of the spectrum of lisfranc injuries. Lisfranc injury x-rays
Management
Depends on the severity of injury, so consult with your orthopedic surgeon to determine operative vs nonoperative management. Patients with stable nondisplaced injuries can be discharged with immobilization in a short leg cast, NWB status, crutches, RICE management and orthopedic surgery follow up.
Keep a high index of suspicion for this injury as missing this injury can lead to deformities, chronic pain and long-term disability.
References
https://coreem.net/core/lisfranc-injuries/
Dixon A, Normal foot x-rays. Case study, Radiopaedia.org (Accessed on 26 Dec 2022) https://doi.org/10.53347/rID-36688
Gaillard F, Lustosa L, Murphy A, et al. Lisfranc injury. Reference article, Radiopaedia.org (Accessed on 26 Dec 2022) https://doi.org/10.53347/rID-1590
https://www.orthobullets.com/foot-and-ankle/7030/lisfranc-injury
Rose NGW, Green TJ. Rosen’s Emergency Medicine: Concepts and Clinical Practice, 49, 623-650.e3. Publisher: Elsevier. Print Publication year: 2022
Sports Medicine for the Emergency Physician A Practical Handbook , pp. 273 – 310. DOI: https://doi.org/10.1017/CBO9781316084328.009[Opens in a new window]. Publisher: Cambridge University Press. Print publication year: 2016
